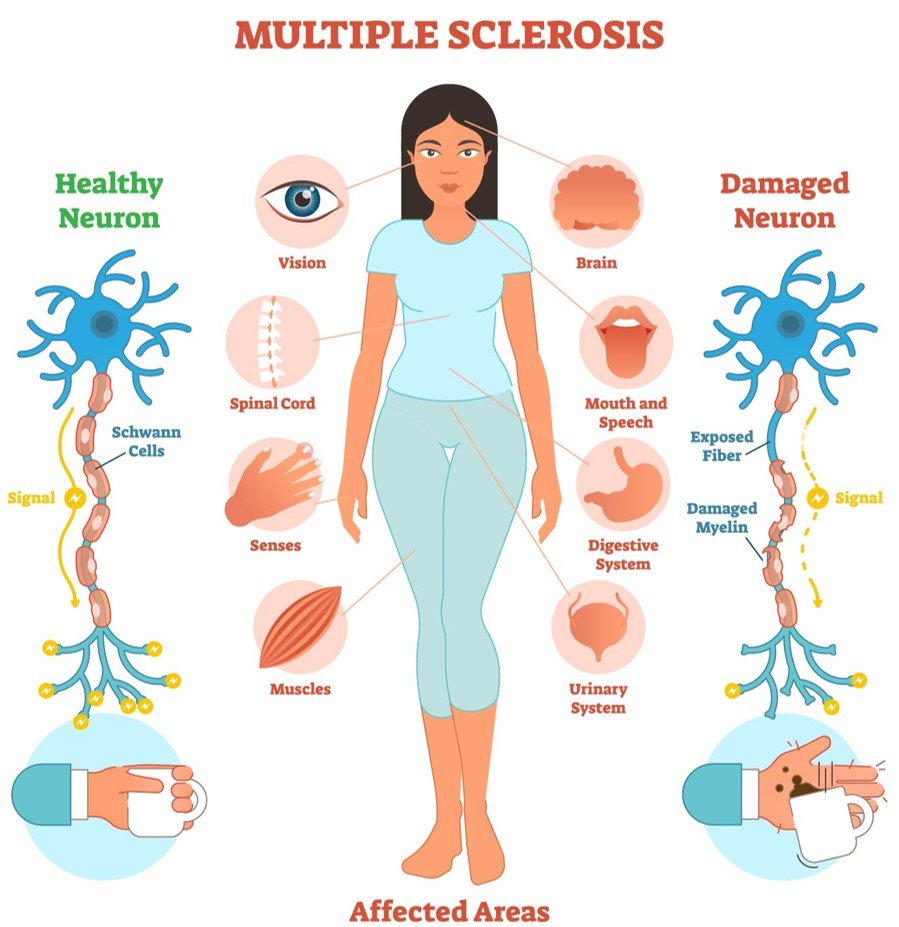
Multiple sclerosis (MS) is a chronic autoimmune disorder affecting the myelin sheath of neurons in the central nervous system (CNS). It is an autoimmune disorder; which means that the immune system mistakenly recognizes the myelin sheath as foreign bodies, attacks the healthy cells, and causes demyelination, neurodegeneration, and inflammation, leading to a number of neurological symptoms. The onset of symptoms usually occurs between 20-40 years of age.
The effect of Multiple sclerosis varies widely and causes significant disability among young adults. Some people with Multiple sclerosis may experience mild symptoms with little disability, whereas others may experience worsening symptoms that will lead to increased disability over time. Despite advancements in research, the exact cause of Multiple sclerosis remains unclear. This blog explores the pathology, symptoms, risk factors, diagnosis, and treatment approaches of MS.
Pathophysiology
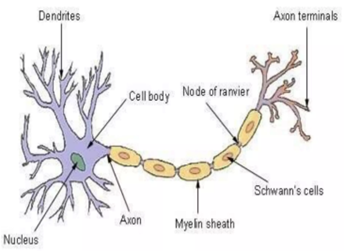
The word “Sclerosis” refers to the areas of scar-like tissue (also called plaques or lesions) that result from the attack on myelin by the immune system. In Multiple sclerosis, the immune system mistakenly attacks myelin in the central nervous system. Myelin is the protective covering (known as the myelin sheath) that coats nerve fibers (axons). It gives the brain’s white matter its whitish appearance and is responsible for communication between neurons.
In Multiple sclerosis, the nerve cell bodies found in the brain’s gray matter are also damaged. With the passage of time, the disease progresses and causes the axonal loss and shrinkage of the cerebral cortex, the neurodegeneration also becomes prominent, contributing to irreversible disability.
Types of Multiple Sclerosis:
Multiple sclerosis presents in different clinical forms, which varies from person to person.
- Relapsing-Remitting Multiple sclerosis (RRMS): This is the most common pattern, affecting about 85% of Multiple sclerosis patients. It is clinically manifested by episodes of symptom exacerbation (relapses) followed by periods of partial or complete recovery (remission) and a stable course between relapses. However the stable course may vary from weeks, months, or even years and then another attack occurs, followed again by a period of inactivity. Most people with Multiple sclerosis are initially diagnosed with this clinical pattern.
- Primary Progressive Multiple sclerosis (PPMS): It is less common and characterized by gradual and nearly continuous worsening of neurological function from onset without distinct relapses.
- Secondary Progressive Multiple sclerosis (SPMS): It begins as Relapsing-Remitting Multiple sclerosis but transitions into a progressive form with accumulated disability.
- Progressive-Relapsing Multiple sclerosis (PRMS): It is a rare form with a gradual decline in function with subsequent superimposed relapses.
Risk Factors and Causes:
The etiology of Multiple sclerosis is multifactorial, involving genetic and environmental factors:
- Genetic Factors: A family history of Multiple sclerosis increases the risk.
- Environmental Factors: Low vitamin D levels, Epstein-Barr virus (EBV) infection, and smoking are linked to increased MS risk.
Clinical Symptoms:
The symptoms of Multiple sclerosis vary depending on the location and size of demyelinated lesions in the Central Nervous System. Common symptoms include:
- Fatigue: One of the most debilitating symptoms, affecting daily activities.
- Visual Disturbances: Changes in the vision, such as double vision or optic neuritis (inflammation of the optic nerve), which causes pain with eye movement and vision loss.
- Motor Dysfunction: Muscle Weakness, often in the arms and legs, spasticity, and impaired coordination can lead to mobility challenges.
- Sensory Symptoms: Numbness, tingling, and pain are frequently reported in the arms, legs, trunk, or face.
- Cognitive Impairment: Memory problems, reduced processing speed, problems concentrating, multitasking, thinking, or learning, and executive dysfunction may develop.
- Bladder and Bowel Dysfunction: Bladder control problems including incontinence, urgency, and bowel dysfunction such as constipation are common.
Diagnosis of Multiple Sclerosis:
For the diagnosis of Multiple sclerosis, no single definite tests are used. It is diagnosed based on clinical evaluation, complete medical history, physical examination, a detailed neurological examination, imaging, and laboratory tests. Key diagnostic tools include:
- Magnetic Resonance Imaging (MRI): MRI scans of the brain and spinal cord are recommended to detect the characteristic white matter lesions in the brain and spinal cord. The patches of lesions can be as small as the head of a pin or as large as a golf ball.
- Lumbar Puncture (CSF Analysis): In Lumbar puncture a sample of cerebrospinal fluid is obtained and examined for proteins and inflammatory cells associated with the disease. The presence of oligoclonal bands in cerebrospinal fluid indicates immune system activity in the Central Nervous System.
- Evoked Potentials: It uses electrodes which are placed on the skin and electrical activity is measured in response to stimuli, detecting demyelination.
- Blood Tests: These are performed to rule out other conditions that mimic Multiple Sclerosis.

Treatment Approaches for Multiple Sclerosis:
There is no cure for Multiple Sclerosis. The treatment approach focuses on reducing the number and severity of relapses, slowing disease progression, and alleviating symptoms.
- Corticosteroids: Corticosteroids such as methylprednisolone are quickly and effective in suppressing the immune system and reducing inflammation. In Multiple Sclerosis, these drugs hasten recovery from MS attacks but do not alter the progression of the disease.
- Disease-Modifying Therapies (DMTs): These medications reduce inflammation by modulating immune response and demyelination, reduce relapse frequency, and delay disease progression:
- Interferon Beta (Avonex, Rebif, Betaseron): Modulates the immune response.
- Glatiramer Acetate (Copaxone): Mimics myelin protein to reduce immune attacks.
- Monoclonal Antibodies (Natalizumab, Ocrelizumab): Target specific immune cells to limit CNS damage.
- Oral Medications (Fingolimod, Dimethyl Fumarate): Modulate immune function and reduce relapses.
- Symptomatic Treatment: Multiple Sclerosissignificantly affects the day to day activities. Therefore, medications and therapies are recommended that focus on reducing the symptoms in the patients of Multiple Sclerosis. Fortunately, many of the symptoms of MS can usually be treated or managed.
- Fatigue Management: Amantadine and lifestyle modifications.
- Spasticity Control: Baclofen and physiotherapy.
- Pain Management: Anticonvulsants and antidepressants.
- Cognitive Rehabilitation: Memory training and cognitive therapy.
- Rehabilitation and Lifestyle Modifications:
- Physical Therapy: Improves mobility and reduces spasticity.
- Diet and Nutrition: Anti-inflammatory diets may benefit MS patients.
- Psychological Support: Counseling and mindfulness techniques enhance mental well-being.
Recent Advancements in Multiple Sclerosis:
Although researchers are unable to identify the exact cause of Multiple Sclerosis several advancements have been made to successfully manage the symptoms and slow the disease progression. New discoveries are aiming to improve MS treatment options and help to reduce MS-related disability.
- Biomarkers: Biomarkers to accurately diagnose MS and monitor disease progression and treatment response, including blood and imaging tests
- Stem Cell Therapy: Hematopoietic stem cell transplantation (HSCT) shows promise in declining the disease progression.
- EBV Vaccine: Given the strong association between EBV and MS, vaccine development is being explored as a preventive measure.
- Neuroprotective Strategies: Research is underway to explore the remyelination therapies and neuroprotective agents.
Conclusion:
Multiple sclerosis remains a complex and chronic autoimmune disorder with diverse clinical manifestations. Although there is no definitive treatment, advancements in disease-modifying therapies and symptomatic treatments have improved the quality of life for patients. Continued research into the pathophysiology, early detection, and therapies focusing on pathways that modify immune system function in the peripheral and central nervous system, repair damaged myelin, or protect neurons from damage holds promise for better management and potential prevention of MS in the future.
FAQs:
- What is multiple sclerosis (MS)?
MS is a chronic autoimmune disease that affects the central nervous system, leading to demyelination, neurodegeneration, and inflammation. - What age group is most commonly affected by multiple sclerosis?
MS usually affects young adults between the ages of 20 and 40. - What are the main types of multiple sclerosis?
The main types are Relapsing-Remitting MS (RRMS), Primary Progressive MS (PPMS), Secondary Progressive MS (SPMS), and Progressive-Relapsing MS (PRMS). - What are some common symptoms of multiple sclerosis?
Common symptoms include fatigue, visual disturbances, muscle weakness, sensory impairments, cognitive issues, and bladder/bowel dysfunction. - Can multiple sclerosis be cured?
There is no cure for MS, but treatments can slow disease progression, manage relapses, and alleviate symptoms.
Reference:
National Institute of Neurological Disorders and Stroke (NINDS). (2025). Multiple sclerosis. Retrieved from https://www.ninds.nih.gov/health-information/disorders/multiple-sclerosis#:~:text=Multiple%20sclerosis%20(MS)%20is%20a,ages%20of%2020%20and%2040.
Davidson, S. (2025). Multiple sclerosis. In Davidson’s Principles and Practice of Medicine (24th ed.). Elsevier.