Cancer – represented by abnormal growth and malignancy – is the third leading cause of death globally. Cancer not only affects millions of individuals each year but also places a substantial burden on healthcare systems, families, and economies. The death ratio of cancer patients is higher in underdeveloped countries with limited resources, greater economic burden, and no access to treatment. However, advances in early detection, prevention strategies, and evolving treatment options have significantly improved survival outcomes and the quality of life for many patients.
Cancer at a glance
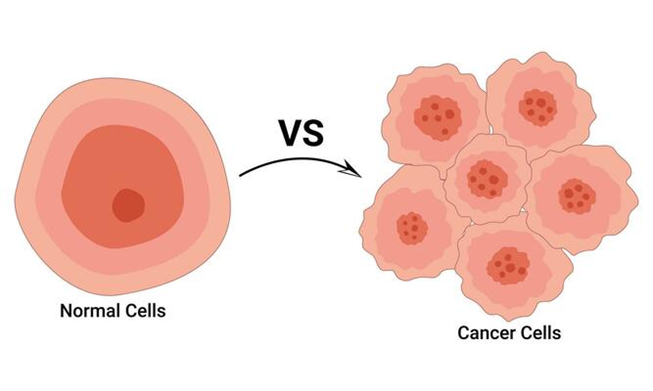
Cancer is a disease characterized by the uncontrolled growth and spread of abnormal cells in the body. Cancer cells grow, divide, and continue to multiply in an unusual manner. Additionally, they invade surrounding tissues or metastasize to distant organs. This abnormal and uncontrolled growth can interfere with essential bodily functions and, if untreated, may become life-threatening.
Cancer is not a single disease but rather a group of over 100 distinct types, each with unique characteristics and behaviors. These types are generally classified based on the organ or tissue of origin—such as breast, lung, colon, prostate, and blood cancers like leukemia. The most common type of cancer is skin cancer; however, cancer of solid organs like the lung, breast, and gastrointestinal tract are prevalent too.
Cancer Development – Carcinogenesis
The development of cancer, or carcinogenesis, truly begins with genetic mutations which disrupt the normal function of genes involved in cell growth and division. These mutations may be inherited or acquired during a person’s lifetime due to environmental exposure, lifestyle factors, infections, or random cellular errors. Over time, such changes result in the transformation of normal cells into malignant tumors capable of spreading and forming secondary growths in other organs.
Common Risk Factors for Cancer
Cancer does not arise from a grain of sand or begin in a vacuum. There are various genetic, lifestyle, and environmental factors that significantly contribute to the development of malignancy. Some of the most common and well-established risk factors include:
- Cigarette smoking is the leading cause of cancer worldwide and is strongly associated with lung, oral, throat, esophageal, bladder, and pancreatic cancers. Even passive exposure to tobacco smoke increases cancer risk. This could be prevented by smoking cessation.
- Unhealthy diet, alcohol consumption, and obesity are other factors that lead to malignancies of the stomach, colon, esophagus, breast, and liver. Exercise, a healthy diet, and lifestyle modifications could reduce the risk.
- Certain viral and bacterial infections play a significant role in cancer etiology.
- Prolonged exposure to ultraviolet (UV) radiation from the sun increases the risk of skin cancer, including melanoma. Occupational exposure to carcinogens like asbestos, benzene, or formaldehyde can lead to lung or blood cancers.
- Family history and genetic mutations have a strong correlation with the development of cancer. Genetic counseling and testing are recommended in such cases.
Therapeutics in Oncology
Cancer treatment is complex and varies with the type, location, stage, and genetic profile of the tumor, as well as the overall health of the patient. The goal of cancer treatment is to eliminate or destroy cancerous cells, prevent their spread, relieve symptoms, and improve the patient’s quality of life. Therapeutics in oncology typically involve one or a combination of the following approaches:
1. Surgery: One of the oldest forms of treatment, surgery is often used to remove localized cancerous masses. It may be curative in early-stage cancers or palliative in advanced cases to reduce symptoms. Surgery is typically needed in three main situations:
- Biopsy: Most cancer diagnoses require a histological or cytological confirmation that can be performed via a tissue biopsy or fine-needle aspiration. These are crucial in providing information on tumor type, grade, and cytology.
- Excision: Surgical removal is the primary curative approach for many localized solid tumors, such as colorectal, breast, and lung cancers. Cure rates are highest when surgery is performed in early stages.
- Palliation: In certain cases where cancer can’t be cured, palliative surgery can quickly and effectively relieve symptoms. Palliative procedures include fixing pathological fractures, decompressing the spinal cord, or managing ulcerating skin lesions. In select cases, surgery may also be used to remove residual masses after chemotherapy or metastases.
2. Chemotherapy: Chemotherapy, a key part of cancer treatment, uses potent drugs that work by killing and stopping the growth of rapidly dividing cancer cells. They don’t specifically target cancer cells, so can also harm normal cells, leading to adverse effects such as nausea, fatigue, hair loss, and immune suppression.
Chemotherapy drugs are grouped based on how they work in the body. Chemotherapy is often given in cycles, usually every 21 or 28 days. Each cycle includes a dose of chemotherapy followed by a recovery period. A full course of treatment usually involves up to six cycles. The exact schedule varies with the type of drugs, how well the patient is responding, and how fast the normal cells recover.
Chemotherapy drugs often have a narrow safety margin, meaning they can easily cause side effects. To help patients tolerate treatment, supportive care is very important. Nausea and vomiting are common but are now better managed using modern anti-nausea drugs like ondansetron along with dexamethasone.

3. Radiation Therapy: Radiation therapy (radiotherapy) uses high-energy radiation to target and kill cancer cells and shrink tumors. It is commonly used for solid tumors, may be curative for certain localized cancers, and may be administered externally or internally (brachytherapy). Radiation therapy is delivered by three methods:
- Teletherapy: Involves application of external beams from a distance via a linear accelerator. Linear accelerators produce high-energy X-rays or electrons to target tumors, damaging cancer cell DNA. To spare normal tissue, CT/MRI and conformal techniques are used to deliver beams precisely.
- Brachytherapy: Involves the direct placement of a radioactive source into or onto the tumor. Brachytherapy allows the delivery of a localized dose of high-energy radiation, which is quite useful in the management of localized cancers (e.g., head, neck, cervix, endometrium).
- Radioisotope injection: Involves the intravenous injection of radioisotopes, e.g., Iodine-131 for thyroid cancer, Strontium-89 for prostate cancer bone metastases.
Fractionation (small daily doses over weeks) is useful as it allows normal cell recovery and enhances the destruction of cancer cells. Radical therapy typically involves 20–30 sessions over 4–6 weeks; palliative care needs fewer. Tumor and normal tissue sensitivity to radiation varies—lymphomas and germ cell tumors are highly sensitive; CNS, bowel, and lungs are vulnerable to damage.
Adverse Effects:
- Localized inflammation (e.g., skin reactions, proctitis, cystitis), that resolves post-treatment.
- Late ADRs that occur after ≥6 weeks (e.g., nerve damage, fibrosis, organ shrinkage).
- Long-term risk: Secondary cancers, especially when combined with chemotherapy.
4. Targeted Therapy
This modern approach uses drugs that target specific molecules involved in the growth, division, and spread of cancer cells, such as HER2 in breast cancer or EGFR in lung cancer. Targeted therapies are generally more precise and have fewer side effects than conventional chemotherapy.
5. Immunotherapy
Immunotherapy is a type of cancer treatment that strengthens the body’s own immune system and helps it recognize and attack cancerous cells. While solid tumors show limited benefit, agents like interferons are effective in melanoma and lymphoma, especially as adjuvants to delay recurrence. IL-2 triggers stronger immune responses but causes significant toxicity. A major success is rituximab, an antibody targeting CD20 on B-cells. It improves response and survival in diffuse large B-cell non-Hodgkin lymphoma and provides palliative benefit in advanced follicular lymphoma.
6. Hormonal Therapy
Hormonal therapy is primarily indicated in hormone-sensitive cancers such as breast and prostate cancer, where it blocks the body’s ability to produce or use certain hormones that fuel tumor growth. ER-positive tumors respond well to anti-estrogen drugs, which reduce relapse and mortality, often with fewer side effects than chemotherapy. Progestogens (e.g., megestrol acetate) are quite effective in endometrial cancer and used in advanced breast cancer when other hormone therapies fail, though their mechanism remains unclear.
7. Stem Cell Transplant
Stem cell transplants are indicated mostly for blood cancers like leukemia or lymphoma. This treatment approach replaces diseased bone marrow with healthy stem cells. Stem cell transplants allow for higher doses of chemotherapy and help regenerate healthy blood cells, significantly improving survival in eligible patients. However, it requires careful patient selection due to risks like infections, graft-versus-host disease (GVHD), and relapse.
Conclusion
Cancer remains one of the leading causes of death globally, but advancements in medical science continue to improve diagnosis, treatment, and survival rates. The development of cancer is often multifactorial. Risk factors include both modifiable and non-modifiable elements. Lifestyle choices such as smoking, alcohol use, poor diet, and lack of physical activity significantly raise cancer risk. Environmental exposures to carcinogens, like radiation or harmful chemicals, also play a role. Additionally, family history, age, infections, and chronic inflammation are critical contributors.
Treatment has evolved from a one-size-fits-all model to more personalized approaches offering hope for patients. Surgical intervention, chemotherapy, and radiation therapy are effective in reducing tumor burden. Immunotherapy and targeted therapy have introduced more precise, less toxic alternatives by focusing on cancer-specific pathways and immune responses.
While no universal cure exists, the prognosis for many cancers has dramatically improved with early diagnosis and combination treatments. Multidisciplinary care, patient education, lifestyle modifications, and access to screening programs are vital in reducing cancer burden globally.
In conclusion, a proactive approach—by understanding and reducing risks, and staying informed about evolving treatments—can significantly influence outcomes. Awareness, timely action, and medical advancements together offer hope in the ongoing battle against cancer.
FAQs:
1. What is cancer and how does it develop?
Answer: Cancer is a disease marked by the uncontrolled growth and spread of abnormal cells. It develops through a process called carcinogenesis, where genetic mutations—either inherited or acquired—disrupt normal cell growth and division. Over time, these mutations cause cells to become malignant, invade nearby tissues, and possibly metastasize to other parts of the body.
2. What are the most common risk factors for developing cancer?
Answer: Common risk factors include:
- Smoking – leading cause globally, linked to lung, oral, and throat cancers.
- Unhealthy lifestyle – including poor diet, alcohol, and obesity.
- Infections – like HPV and hepatitis B/C.
- UV and carcinogen exposure – from sunlight and chemicals like asbestos.
- Genetic predisposition – family history and inherited mutations.
Most of these risks are preventable through lifestyle modifications and early interventions.
3. How is cancer diagnosed and treated surgically?
Answer: Diagnosis typically involves biopsies or fine needle aspirations to confirm cancer type and grade. Surgery is used to excise tumors in early stages, to relieve symptoms in advanced cases (palliative surgery) or to remove residual masses post-chemotherapy.
4. What are the main treatment options for cancer besides surgery?
Answer: Other key treatments include:
- Chemotherapy – targets rapidly dividing cells, often in cycles.
- Radiation Therapy – uses high-energy beams or radioactive sources.
- Targeted Therapy – attacks specific cancer-related molecules.
- Immunotherapy – enhances the body’s immune response.
- Hormonal Therapy – blocks hormones in hormone-sensitive cancers.
- Stem Cell Transplant – used for blood cancers to restore healthy marrow.
5. Can cancer be cured or only managed?
Answer: Some cancers, especially when diagnosed early, can be completely cured, particularly through surgery or combined therapies. Others may be managed long-term with a focus on controlling growth, relieving symptoms, and improving quality of life. Advances in personalized medicine and targeted therapies have significantly improved outcomes, even in advanced cases.
References:
- Davidson’s Principles and Practice of Medicine. 24th ed. Edinburgh: Elsevier; 2022.
- National Cancer Institute. Types of Cancer Treatment. [Internet]. Available from: https://www.cancer.gov/about-cancer/treatment/types





