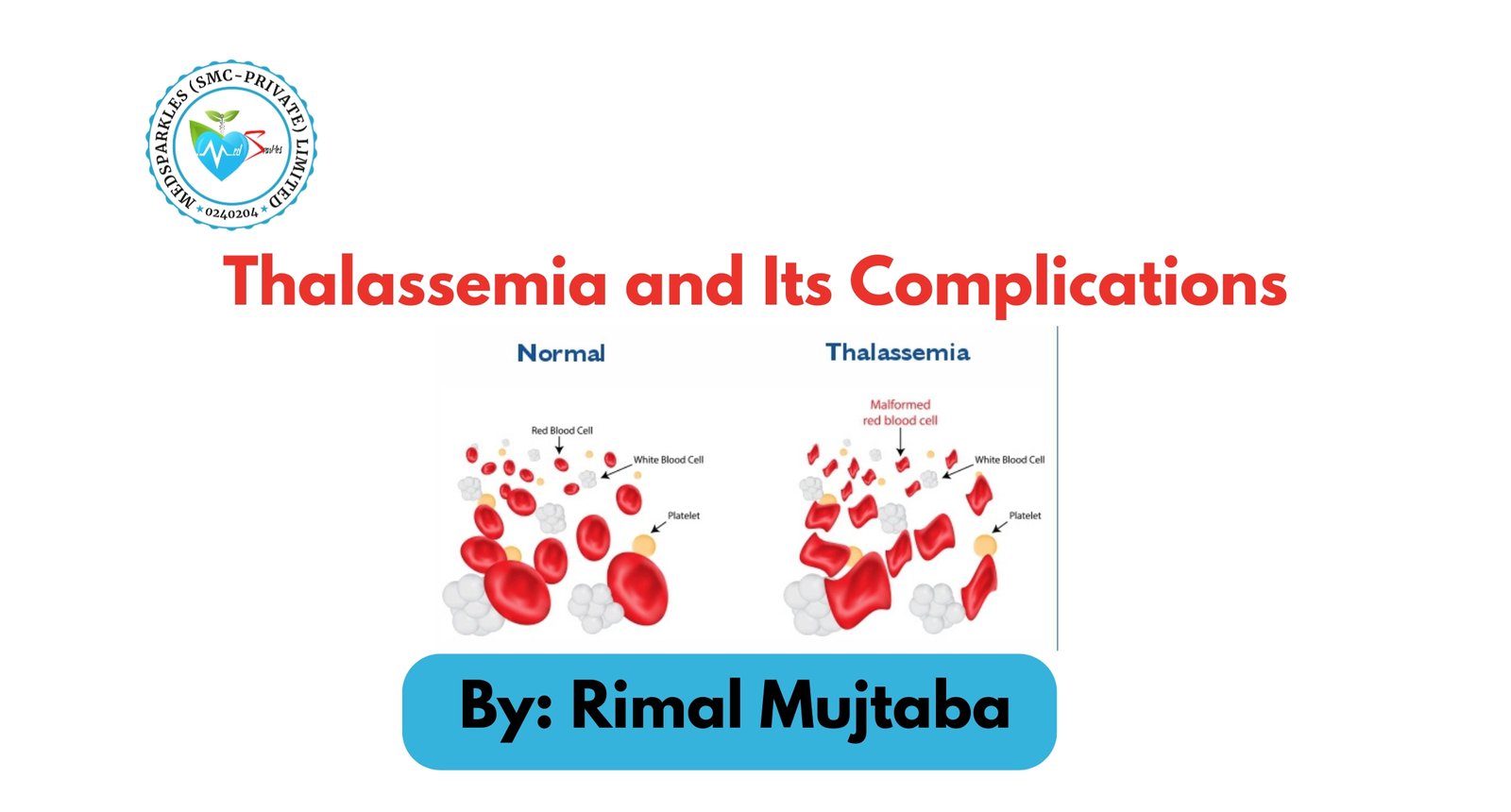
Thalassemia is an inherited blood disorder that causes the body to make fewer healthy red blood cells and less hemoglobin than normal. Hemoglobin is an iron-rich protein, present in red blood cells, that carries oxygen to all parts of the body and removes carbon dioxide from the body through the lungs. Being an inherited disorder, it also passes from parents to children through genes. The patients of thalassemia can have mild or severe anemia, and the disorder can be diagnosed in early childhood; and mainly considered a lifelong condition.
Thalassemia and Its Types:
Normal hemoglobin has four protein chains—two alpha and two beta. The two major types of thalassemia, alpha and beta, are named after defects in these protein chains.
Alpha Thalassemia:
Four genes (two from each parent) are needed to make enough alpha protein chains. Alpha thalassemia trait occurs if one or two of the four genes are missing. If more than two genes are missing, moderate to severe anemia occurs. It is a silent carrier and can be named in multiple ways. For example,
- Alpha Thalassemia Minor/Thalassemia Trait: It is a genetic disorder characterized by small red blood cells, often asymptomatic with or without mild anemia.
- Alpha Thalassemia Major/Hydrops Fetalis: It is the most severe form of alpha thalassemia, and babies who have this disorder usually die before or shortly after birth.
- Hemoglobin H disease: a form of alpha thalassemia caused by a defect in the hemoglobin protein.
Beta-Thalassemia:
Two genes (one from each parent) are needed to make enough beta protein chains. Beta thalassemia occurs if one or both genes are altered. Based on the severity of the disease, beta-thalassemia can be further classified as;
- Thalassemia major, or Cooley’s anemia. The severe form of beta thalassemia is known as thalassemia major or Cooley’s anemia.
- Beta thalassemia minor, also called beta thalassemia trait, involves one faulty beta-globin gene, causing a mild or no anemia
- Beta thalassemia intermedia causes moderate anemia due to reduced beta-globin production.
- Beta-plus (ß+) thalassemia is when the body produces a reduced but not absent amount of beta-globin.
- Mediterranean anemia: occurs when the body produces insufficient or abnormal hemoglobin.
Signs and Symptoms:
Anemia can be a major symptom in patients suffering from thalassemia. However, the severity of symptoms is associated with the severity of symptoms.
- No symptoms:
Usually, alpha thalassemia is asymptomatic in nature, mainly because the lack of alpha globin protein is so minor that the body’s hemoglobin works normally.
- Mild Anemia:
People might experience little tiredness—a major sign of mild anemia.
- Moderate Anemia:
Moderate anemia can be associated with other health issues such as slower growth, delayed puberty, bone problems, and spleen enlargement.
- Severe Anemia:
People with hemoglobin H disease or beta-thalassemia major can experience severe anemia. The major signs include a pale, dull appearance, poor appetite, dark urine, bone problems, enlarged spleen, and delayed puberty.
Complications:
Better treatment options are available to treat moderate and severe signs and symptoms of thalassemia that allow people to live much longer. But these people must cope with complications of these disorders that occur over time. A few of the complications are listed as:
Heart Diseases: Regular blood transfusions are a standard treatment for thalassemia. Transfusions can cause iron to build up in the blood (iron overload). This can damage organs and tissues, especially the heart and liver. Heart disease caused by iron overload is the main cause of death in people who have thalassemia. Heart disease includes heart failure, arrhythmias (irregular heartbeats), and heart attacks.
Infection: Among people who have thalassemia, infections are a key cause of illness and the second most common cause of death. People who have had their spleens removed are at even higher risk because they no longer have this infection-fighting organ.
Osteoporosis: Many people who have thalassemia have bone problems, including osteoporosis. This is a condition in which bones are weak and brittle and break easily.
Liver Disease: Repeated blood transfusions can lead to liver damage from infections, like Hepatitis C, and iron overload. Chronic inflammation and scarring (fibrosis) from iron buildup can progress to liver cirrhosis and ultimately lead to liver failure.
Endocrine Complications: Thalassemia-associated endocrine complications include: Diabetes mellitus, Hypothyroidism, Hypogonadism, Growth retardation, etc.
Enlarged Spleen and Liver: These organs enlarge to compensate for the anemia and due to iron deposition.
Conclusion
In conclusion, thalassemia is more than just a genetic blood disorder—it’s a lifelong challenge that demands proper medical care, emotional support, and community assistance. Its complications, ranging from severe anemia and organ damage to growth delays and iron overload, emphasize the importance of early diagnosis and consistent treatment. While medical advancements like blood transfusions and iron chelation therapy have improved patient outcomes, awareness and education remain crucial in preventing new cases through genetic counseling and carrier screening.
‘‘Thalassaemia is more than a clinical condition; behind every statistic is a person with unique experiences, aspirations, and challenges’’
FREQUENTLY ASKED QUESTIONS
Q1. What complications can thalassemia cause?
It can lead to iron overload, bone deformities, and delayed growth.
Q2. Can thalassemia be prevented or cured?
Prevention is possible through genetic screening, though treatment focuses on symptoms.
Q3. How is thalassemia diagnosed?
Thalassemia is diagnosed through blood tests that assess hemoglobin levels and genetic analysis to confirm the mutation.