Abstract
In order to relieve the climacteric symptoms of menopause, Hormone Replacement Therapy (HRT) is given. After a report from the Women’s Health Initiative the use of HRT is reduced because it is linked with increased risk of breast cancer. This risk appears to be noticeable after 5 years of HRT use .The risk of breast cancer associated with estrogen receptor- positive is increased as compared to estrogen receptor-negative. A clear risk is seen for current uses of combined estrogen/progestogen pills, but this returns to normal after treatment cessation. The factors that are responsible for increasing the risk of breast cancer are initiation of hormone therapy right after menopause, high mammographic breast density and a lean body mass. This review demonstrated the biological effects of estrogen and progesterone on expansion of breast cancer cells on the basis of research and trials to improve functions of hormones as a safety of MHT.
Introduction
During menopause, oestrogen level is decreased that is injurious to health and causes breast cancer. Women take the medication to replace the oestrogen; this type of therapy is known as hormone replacement therapy.
The risk of breast cancer depends upon the type of hormone therapy, its duration, dosage and health of the patient. On large scale, epidemiological and clinical studies on oestrogen and breast cancer are determined to be interlinked. (Bush, Whiteman, & Flaws, 2001)For example after menopause chances of breast cancer reduced ,the reduced risk of breast cancer in ovariectomized women and those with early natural menopause, and the efficacy of antiestrogen drugs in preventing and treating breast cancer . Moreover, following the use of hormone replacement therapy high risk of breast cancer occurred.
In 1997, the pooled analysis originating from the USA, with limited data, showed that the increased risk of breast cancer occurs by using HRT. Furthermore, by delaying menopause risk of breast cancer can be reduced.
Worldwide, from the past two decades regimen prescription opposed by progestin has increased. In the USA, medroxyprogesterone-acetate is used as progestin, which resembles natural progesterone and is administered either cyclically or continuously.(Canonico, 2015) In Europe the predominant regimen prescribed is 17-b-oestradiol that is taken by testosterone-derived progestin mainly which include north testosterone acetate (NETA) or levonorgestrel (LNG); while the less androgenic progestin MPA is used to a lesser extent.
Regarding progesterone a study showed an inverse relationship between serum level in luteal phase and successive diagnosis of breast cancer. Thus the drug replacement regime is used as a continuous basis. Due to traditional differences of prescription practices in USA and Europe; it has been difficult to determine the risk of breast cancer according to the type of progestin or treatment.
In 1993, a case-control study in Denmark found that current use was the highest in the age group 53–54 years (30%), but only 2/3 of cases were reported with combined treatment of oestrogen and progestin. In 1994, 24% of 54-year-old women were using HRT in Sweden.
In Norway, 1/3 of Norwegian women aged 60 years or older are current or past users of HRT .The recent use of HRT has been estimated in a random sample of Norwegian increased from 16.3% in 1994 to 19.1% in 1996. (Harper-Harrison & Shanahan, 2022) Hormone replacement therapy can increase the chances of disease reversal if you have history of breast cancer. Because of this doctors don’t recommend the use of hormone replacement therapy.
Before knowing the link between hormone replacement therapy and breast cancer, women use to take for ease in menopausal symptoms. But after 2022, the use of HTN reduced dramatically due to its adverse effect.
The aim of the present review is to evaluate and summarize the epidemiological evidence concerning the risk of breast cancer conferred by different HRT treatment regimens that focus on the combined oestrogen plus progestin treatment. In this review you will study the effect of progesterone in body, Cause of breast cancer, side effects, precaution and combination medication used for treatment.(Ross, Paganini-Hill, Wan, & Pike, 2000)
Why this medication is prescribed?
Estrogen and progestin are two female sex hormones.
In case of menopause, the combination of two hormones including estrogen and progestin prescribed to treat certain symptoms. In case of hormone replacement therapy , it works by replacing estrogen hormone which is no longer being made by the body after menopause in women .
Estrogen reduces feelings of warmth in the upper body and periods of sweating and heat (hot flashes), vaginal symptoms (itching, burning, and dryness) and difficulty with urination, but it does not relieve other symptoms of menopause such as nervousness or depression.(van Leeuwen et al., 1994)
Estrogen is essential in preventing thinning of the bones (osteoporosis) in menopausal women. Progestin is added to estrogen in hormone replacement therapy to reduce the risk of uterine cancer in women who still have their uterus.
In hormone replacement therapy, progestin is added to the estrogen to reduce the risk of hyperplasia as well as adenocarcinoma of the endometrium. Studies have shown that there are considerably increases the risk of endometrial hyperplasia and cancer due to the administration of estrogens alone to non- hysterectomized women. (Trabert, Sherman, Kannan, & Stanczyk, 2020)
How to use medicine?
- Hormone replacement therapy is available as a tablet to take by mouth.
- It is usually taken once a day.
- Take it around the same time every day this will help you remember to take hormone replacement therapy.
- Take the medicine according to your prescription follow the directions mentioned on label.
- Ask your doctor or pharmacist to explain any part you do not understand.
- Take the appropriate amount of dose as prescribed.
- Do not stop taking this medication without talking to your doctor.(Spaulding, 1994)
Why progesterone is included in Hormone Replacement Therapy?
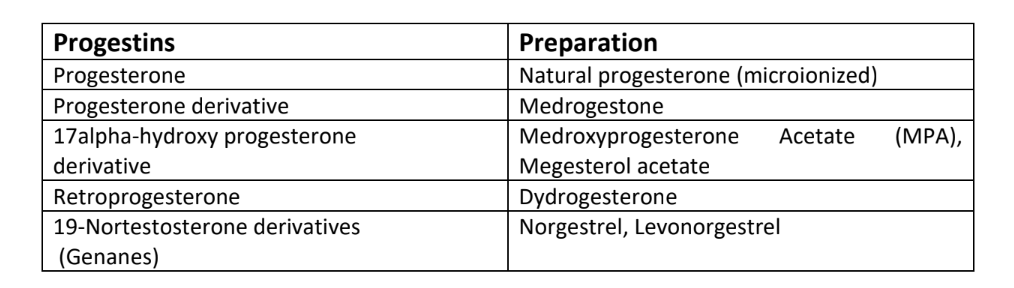
Classification of Progestins used in HRT
Hormone Replacement Therapy & Risk of Breast Cancer
Hormone Replacement Therapy increases the risk of breast cancer but people who uses combined HRT both progestin and estrogen is at higher risk of breast cancer. Tibolone is associated with increased risk of Breast Cancer than vaginal estrogens. Risk of Breast Cancer is slightly increases when you take HRT for 1 year or less. But when you take HRT for long time greater the risk and longer they last.(Lobo, 1992)
From person to person the risk of Breast Cancer due to HRT varies. For example, your age when you are taking first human replacement therapy. General health of person and medicines that you have already use such things have greater impact on risk of Breast Cancer. People who use HRT before or soon after menopause are at greater risk of Breast Cancer than those who use later Risk of Breast Cancer lasted for more than 10 years after women stopped taking HRT.(Poggio et al., 2022)
Difference between various Hormone Replacement Therapies and Risk of Breast Cancer
HRT regimen relies on stages of menopause whether it is early stage or postmenopausal stage. Mainly 2 type of regimen are in process that is cyclical or continuous combined HRT. Data based study provide appropriate results on both sequential and continuous combined regimen. Chances of breast cancer are more with ccHRT mainly when used for a long period. Comparative findings on estrogen level are quite difficult in different countries because of variation in estrogen level. (Campagnoli, Clavel-Chapelon, Kaaks, Peris, & Berrino, 2005) The risks are more distinct and consistent in studies conducted in Northern Europe than in US. This might happen in US because sequential method has been more appreciative in women. In Northern Europe, the daily dose of norethisterone acetate, 1mg was same in both therapy and twice in case of monthly commutative dose. (Harper-Harrison & Shanahan, 2022) Although is US, combined regimen is 2.5 mg lower than sequential 5-10mg not differ greatly in dose. Cross sectional study in Us found an increase in proliferation in women using breast biopsies. The increase in proliferation was passable in early stages and exacerbate over years. Continuous combined regimen increase the risk of Breast cancer due to no epithelial sloughing and natural progesterone they do not have any breast cancer issues. (Ross et al., 2000)
Estrogenic Effects of Progestin:
Vitro studies has shown that the progestin derived from 19-Nortestesterone exerts a estrogen like proliferative effect on the BC cell lines. This effect is mediated by the decreased 5 alpha metabolites which interact with alpha and beta estrogenic receptors. One might be able to conceive progestin with androgenic activity that stimulate the BC cell proliferation through interaction with the androgen receptors.(Pasqualini et al., 1996)
Effects of Progestin on Cancer Cell Enzymes:
An estrogen sensitive cancer cell expresses an enzyme that enables to produce the estrodiol from the circulating androgens, estrone sulfate and estrone. Among these the most important are aromatase 17-beta hydroxysteroid dehydrogenases and estrone sulfatas . Vitro studies indicate that the progestin can inhibit the activity of estrone sulfatase and influence the activity of 17 beta-HSD, decreasing the formation of estradiol.(Markiewicz, Hochberg, & Gurpide, 1992). In experimental conditions MPA appear to be different from progesterone and other progestin in being able to promote the reductive transformation of the estrone into estradiol via 17 beta-HSD. This might be important in women with high level of estrone, occurs when the oral estrogen containing HRT is employed. (Jeng, Parker, & Jordan, 1992)
Side Effects of Progesterone in Hormone Replacement Therapy
Side effects from hormone replacement treatment are possible. If any of these symptoms are severe or do not go away, let your doctor know right once;
- Headache
- Stomach upset
- Stomach cramps and bloating
- Vomiting and diarrhea
- Appetite and weight changes
- Change in sex drive and ability
- Nervousness
- Black and brown skin patches
- Breast tenderness, enlargement or discharge
- Changes in menstrual flow (Warren & Shantha, 1999)
Some adverse effects can be very harmful. Although the following signs and symptoms are unusual, if you notice any of them or any of the ones in the IMPORTANT WARNING section, call your doctor right away,
- Dual perception
- Acute stomach discomfort
- Eyes or skin that have a yellow tint
- Severe depression of the mind
- Uncommon bleeding
- Excessive fatigue, weakness, or lack of energy fever loss of appetite
- Urine with a dark color
Endometrial cancer and gallbladder disease risk may rise with hormone replacement therapy. The dangers of using this drug should be discussed with your doctor. Other negative effects of hormone replacement therapy are possible. If you experience any strange issues while taking this medicine, contact your doctor right away.
What should I be aware of about the handling and disposal of this medication?
Keep this medication tightly closed in the original container and out of the reach of children. Keep it in a cool, dry place away from heat and moisture.
Unused prescriptions must be disposed of carefully to prevent pets, kids, and other people from ingesting them. You should not, however, dispose of this medication in the toilet. Instead, utilizing a medicine take-back program is the easiest approach to get rid of your medication. To find out about take-back program in your area, speak with your pharmacist or the garbage/recycling department in your city.
It is essential to keep all medicine carefully concealed and reach of kids as numerous compartments, (for example, week after week pill minders and those for eye drops, creams, patches, and inhalers) are not kid safe and little youngsters can open them without any problem. To safeguard small kids from harming.
Overdose of Progesterone in Hormone Replacement Therapy
Estrogen overdose
Estrogen is a hormone produced by females. The following is a list of things to do if you find yourself in a situation where you need to use the restroom. This can happen by chance or on purpose.
Symptoms of estrogen overdose include
- Breast sensitivity
- Urine discoloration
- Emotional shifts
- Drowsiness
- Excessive vaginal bleeding (2 to 7 days after overdose)
- Retention of fluid
- Headache
- Vomiting and nausea
- Rashes on the skin
Treatment of overdose include
- Reduce your body fat percentage.
- Reduce stress.
- Eat a healthy diet: Eating a low-fat, high-fiber diet with little processed sugar can help your liver process estrogen more easily.
- Limit your alcohol consumption: Avoiding or drinking in moderation can help your liver break down estrogen.
Progesterone overdose
Using this medicine in high doses for an extended period of time, or in combination with estrogen, may increase your risk of heart attack, stroke, blood clots, or dementia. Discuss these risks with your doctor. If you smoke, you are at a higher risk of developing heart disease or having a stroke as a result of this medication.
Symptoms of progesterone overdose include
- Heart attack
- Stroke
- Blood clots
- Dementia
Treatment of overdose include
Taking estrogen with progesterone lowers your risk of endometrial cancer, the lining of the uterus, when compared to taking estrogen alone. While progesterone is most commonly used as a form
Conclusion
It is now clear that combined use of estrogen/progestin preparations notably increase the risk of breast cancer in current users.
The greater risk breast cancer associated with the use of HRT preparations containing estrogen and synthetic progestin seems in all likelihood due to the regimen and to the kind of progestin used.
It is therefore suggest that when HRT is suggested, preparations containing progesterone and not a synthetic progestin should be used. In this way the risk of endometrial cancer is minimized without increasing the risk of Breast cancer.
References
Brown, K. F., Rumgay, H., Dunlop, C., Ryan, M., Quartly, F., Cox, A., . . . Hounsome, L. (2018). The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. British journal of cancer, 118(8), 1130- 1141.
Bush, T. L., Whiteman, M., & Flaws, J. A. (2001). Hormone replacement therapy and breast cancer: a qualitative review. Obstetrics & Gynecology, 98(3), 498-508.
Campagnoli, C., Clavel-Chapelon, F., Kaaks, R., Peris, C., & Berrino, F. (2005). Progestins and progesterone in hormone replacement therapy and the risk of breast cancer. The Journal of steroid biochemistry and molecular biology, 96(2), 95-108.
Canonico, M. (2015). Hormone therapy and risk of venous thromboembolism among postmenopausal women. Maturitas, 82(3), 304-307.
Harper-Harrison, G., & Shanahan, M. M. (2022). Hormone Replacement Therapy StatPearls [Internet]: StatPearls Publishing.
Jeng, M.-H., Parker, C. J., & Jordan, V. C. (1992). Estrogenic potential of progestins in oral contraceptives to stimulate human breast cancer cell proliferation. Cancer Research, 52(23), 6539-6546.
Judd, H. L., Mebane-Sims, I., Legault, C., Wasilauskas, C., Johnson, S., Merino, M., . . . Barnabei, V. (1996). Effects of hormone replacement therapy on endometrial histology in postmenopausal women: the Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. Jama, 275(5), 370-375.
Lobo, R. A. (1992). The role of progestins in hormone replacement therapy. American journal of obstetrics and gynecology, 166(6), 1997-2004.
Markiewicz, L., Hochberg, R. B., & Gurpide, E. (1992). Intrinsic estrogenicity of some progestagenic drugs. The Journal of steroid biochemistry and molecular biology, 41(1), 53-58.
Pasqualini, J., Chetrite, G., Blacker, C., Feinstein, M., Delalonde, L., Talbi, M., & Maloche, C. (1996). Concentrations of estrone, estradiol, and estrone sulfate and evaluation of sulfatase and aromatase activities in pre-and postmenopausal breast cancer patients. The Journal of Clinical Endocrinology & Metabolism, 81(4), 1460-1464.
Poggio, F., Del Mastro, L., Bruzzone, M., Ceppi, M., Razeti, M. G., Fregatti, P., . . . Franzoi, M. A. (2022). Safety of systemic hormone replacement therapy in breast cancer survivors: a systematic review and meta-analysis. Breast Cancer Research and Treatment, 1-7.
Ross, R. K., Paganini-Hill, A., Wan, P. C., & Pike, M. C. (2000). Effect of hormone replacement therapy on breast cancer risk: estrogen versus estrogen plus progestin. Journal of the National Cancer Institute, 92(4), 328-332.
Spaulding, L. B. (1994). Endometrial ablation for refractory postmenopausal bleeding with continuous hormone replacement therapy. Fertility and sterility, 62(6), 1181-1185.
Trabert, B., Sherman, M. E., Kannan, N., & Stanczyk, F. Z. (2020). Progesterone and breast cancer. Endocrine reviews, 41(2), 320-344.
van Leeuwen, F. E., Van den Belt-Dusebout, A., Benraadt, J., Diepenhorst, F., Van Tinteren, H., Coebergh, J., . . . Schouten, L. (1994). Risk of endometrial cancer after tamoxifen treatment of breast cancer. The Lancet, 343(8895), 448-452.
Warren, M. P., & Shantha, S. (1999). Uses of progesterone in clinical practice. International journal of fertility and women’s medicine, 44(2), 96-103.




