Chronic pain is the most common health problem among older adults. It is a persistent and often debilitating reality for many older adults, significantly influencing their quality of life. While it’s easy to assume pain is just an inevitable part of the aging process, the truth is that chronic pain can be effectively managed, reduced, and in some cases, even prevented from worsening. The key lies in a proactive approach that integrates medical expertise, lifestyle adjustments, mental health support, and a robust social network.
Chronic pain is more than just a sensory event; it has affective (emotional responses to pain), cognitive (attitudes and beliefs about pain), behavioral (for example, behaviors manifested in response to pain by patients and their family members or caregivers), as well as sensory components (for example, quality, location, temporal pattern). Assessing the presence and severity of pain captures only a small part of the pain experience. All older patients with chronic pain should undergo a comprehensive pain assessment.
Common Causes of Chronic Pain:
There is a common belief that chronic pain is an unavoidable consequence of getting older. Chronic pain does have a high prevalence in the older population, estimated to be over 50%, with 70% of older individuals endorsing pain in multiple sites. The most prevalent painful conditions affecting older adults are arthritis-related, although the incidence of chronic systemic disease can also result in pain.
· Cancer-related pain
· Central poststroke pain
· Chronic post-surgical pain
· Diabetic peripheral neuropathy
· Fibromyalgia
· Myofascial pain
· Osteoarthritis
· Peripheral vascular disease (ischemic pain)
· Postherpetic neuralgia (shingles)
· Spinal canal stenosis
· Trauma-related pain (ex. Hip fracture)
Importance of Early Diagnosis and Regular Assessments:
One of the biggest challenges in treating chronic pain is recognizing it early. Because many seniors believe pain is a normal part of aging, they may downplay or ignore symptoms. Conversely, some fear additional medical procedures or costs. However, delaying treatment can exacerbate the underlying condition, potentially leading to greater discomfort, reduced mobility, or complications.
Early diagnosis and intervention often involve a thorough evaluation that includes medical history, a physical exam, and potentially imaging tests like X-rays, MRIs, or CT scans. Seniors might also be referred to specialists—ranging from orthopedists to neurologists—depending on the suspected cause of pain. Identifying the root causes allows healthcare providers to customize a comprehensive pain management plan.
Lifestyle Modifications That Help Reduce Pain:
Beyond formal treatments, simple lifestyle changes can yield substantial benefits for seniors dealing with chronic pain.
Exercise and Movement:
The key is consistency and moderation. Overexertion may worsen pain, so seniors should aim for gradual progress. Consulting with a healthcare provider to develop a safe routine is highly recommended, especially for those with underlying cardiac or orthopedic conditions.
Weight Management and Nutrition:
Carrying extra weight can intensify joint pain, particularly in weight-bearing areas like the knees and hips. A balanced diet rich in protein, vitamins, and minerals (especially calcium and vitamin D) can boost muscle and bone health. Resources like free meal delivery services may support seniors who struggle to shop or cook, ensuring they receive nutrient-dense meals.
Mind-Body Techniques:
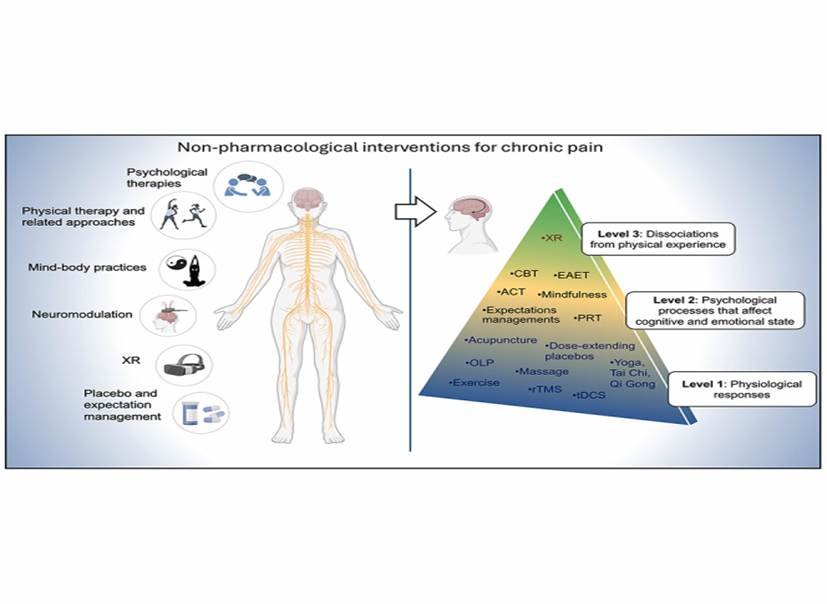
Chronic pain has a strong psychological component. Techniques like guided imagery, meditation, and breathing exercises can alleviate stress and anxiety, which often exacerbate discomfort. Some seniors also benefit from cognitive-behavioral therapy (CBT), which teaches practical skills for coping with pain flares, negative thought patterns, and emotional distress.
Spiritual practices like attending religious services or seeking spiritual support may also help individuals find comfort and resilience in the face of persistent discomfort.
Medication Options:
In cases of severe or unmanageable pain, doctors might prescribe opioids, muscle relaxants, or stronger NSAIDs. Opioids such as oxycodone and morphine can be highly effective but carry a risk of dependence and severe side effects like drowsiness, constipation, or respiratory depression. Physicians often recommend a careful “start low and go slow” approach, accompanied by regular check-ups to assess efficacy and side effects.
Adjuvant medications, like antidepressants or anticonvulsants (e.g., gabapentin, pregabalin), can also assist in managing neuropathic pain. These drugs modulate nerve signals and may provide relief when standard analgesics prove insufficient.
Topical creams or patches containing capsaicin or lidocaine can offer localized relief with fewer systemic side effects. Meanwhile, corticosteroid injections directly into inflamed joints can reduce swelling and pain for several weeks or months.
Seniors receiving injections for chronic conditions such as arthritis should maintain open communication with healthcare providers regarding frequency, side effects, and potential risks like joint damage or infection.
Embracing a Holistic Perspective on Pain:
Chronic pain doesn’t solely reside in the body—it also affects emotions, mental health, and daily life. A holistic viewpoint recognizes this interconnectedness, prompting a blend of medical treatments, therapeutic interventions, emotional support, and lifestyle modifications.
Medical advances continue to bring new pain management solutions, from regenerative therapies to innovative implants. However, the human element—understanding pain’s emotional weight, nurturing relationships, and fostering resilience—remains equally crucial. By harmonizing these aspects, seniors can find meaningful, long-lasting relief.
Conclusion:
Chronic pain in seniors is a multi-faceted challenge, shaped by physical, emotional, and social factors. While it can significantly disrupt daily life, a well-rounded pain management plan offers hope for improved comfort and autonomy. From medication regimens and therapeutic exercises to psychological coping strategies and healthcare support, multiple pathways exist to reduce suffering and enhance quality of life.
FAQs:
1. What is the most common cause of chronic pain in older adults?
Arthritis is the most frequent cause, leading to joint stiffness and long-term discomfort.
2. Can exercise help reduce chronic pain in seniors?
Yes, gentle activities like walking or stretching improve mobility and decrease pain.
3. Are pain medications safe for older adults?
They can be safe when used under medical supervision and at the lowest effective dose.
4. When should an older adult see a doctor for chronic pain?
If the pain lasts over three months or affects daily activities, a medical evaluation is needed.
References:
1. Reid, M. C., Eccleston, C., & Pillemer, K. (2015). Management of chronic pain in older adults. BMJ (Clinical Research ed.), 350, h532.
2. World Health Organization. Guidelines on Integrated Care for Older People (ICOPE), 2020.
Image credit: pmc.ncbi.nlm.nih.gov





