Pediatric patients are different from adults. They are those playful creatures that always think of cherishing naughty things. Pediatrics belongs to the age group that is not fully mature. Their organs are still under development. Based on age, they are classified into further subtypes like neonate, infant, toddler, child, and adolescent. After the adolescent level, they become adult. The following picture illustrates various stages of a child’s development from infancy to adulthood.
Fig 1: Picture depicting different levels of pead development up to adulthood.
ANTIBIOTIC USAGE IN PEDIATRICS
Unlike adults, children have not developed immunity to combat all the seasonal and other bacterial infections. Their skin is also very soft & permeable, which makes them susceptible to gram-positive & gram-negative bacterial infections. According to the Pediatric Clinical Classification System by the USA, during the stages of pediatric development, the children endure different clinical challenges like fever, pneumonia, respiratory failure, asthma, bronchiolitis & otitis media & much more. To withstand & overcome these conditions, they need to be treated with antibiotics. A range of antibiotics may be used to treat such kind of infections in children. These antibiotics include Cefixime (for the treatment of gastroenteritis caused by Salmonella, Shigella sp.), Ceftriaxone, Azithromycin (for mitigating pneumonia), Clindamycin (used prophylactically for Streptococcal infections in lungs), Gentamicin (for attenuating UTI, RTI), Erythromycin (for skin infections), Vancomycin (for alleviating lower RTI, skin, bone infections), Linezolid (for mitigating mycobacterial infections), Piperacillin/Tazobactum (for curing neutropenic children with fever), Cefoperazone/ Sulbactum (for alleviating mild-moderate bacterial infections), Ampicillin (for lessening UTI & pharyngitis), Cefotaxime (for curing meningitis, pneumonia), Levofloxacin (for the treatment of anthrax infection), Carbapenem/Imipenem (for treating multi-drug resistant infections) and Colistin (for attenuating infections originated by gram negative bacteria). These antibiotics are used to treat a broad spectrum of gram-positive & gram-negative bacterial infections. Some of the common brands of antibiotics are shown in the following figure.


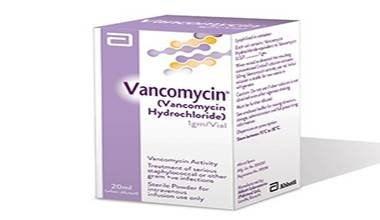
Fig 2: Some common brands of antibiotics.
MICROBIAL SPECIES THAT HAVE GAINED RESISTANCE
The microbial species that are responsible for the genesis of bacterial infections in pediatrics, as well as the adult population, are Salmonella typhi, Salmonella paratyphi, Staphylococcus sp., E. coli, Staphylococcus aureus, Streptococcus sp., Klebsiella pneumonia, Pseudomonas aeruginosa, Enterobacter sp., Enterococci sp., Candida sp. The presence of mycobacterial infections due to these species in the pediatric population was further confirmed in a study organized by an Indian microbiologist. The following figures depict the role of these microorganisms in the outspread of bacterial infections in the pediatric population.
Fig 3: Cultures of bloodstream infections revealing causative organisms from the pediatric OPD ward in India.
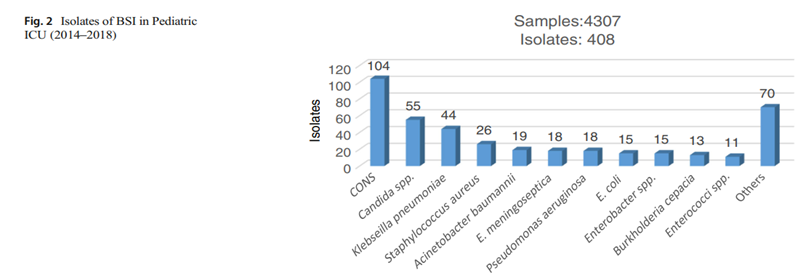
Fig 4: Cultures of bloodstream infections depicting causative organisms from the pediatric ICU Ward in India.
The emergence of resistance to antibiotics in microbes, either due to overuse or misuse, was found by Wattal et all in a study organized in 2019. This resistance is portrayed in the following table.
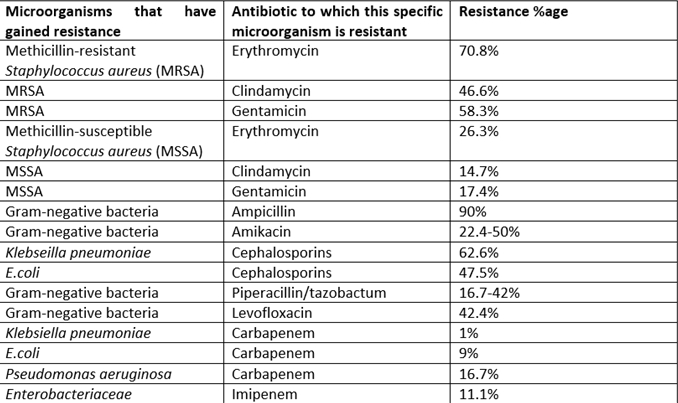
Table 1: Resistance percentage of different microorganisms against specific antibiotics.
POTENTIAL WAYS FOR TACKLING AMR
In one of the studies organized by an Italian scientist in 2023, suggested that antimicrobial stewardship strategies must include point-of-care testing for urinary tract infections in the pediatric population. This type of testing differentiates between bacterial & viral infection & thus the resistance that is being developed due to the overuse of antibiotics can be prevented. The independent medication use of antibiotics by parents for their children can also be the main cause of antimicrobial resistance in children. So, without the proper diagnosis & guidance by the healthcare practitioner, antibiotics should not be used in pediatrics.
It is estimated that 50% of all antimicrobial use is unnecessary or inappropriate.
A South Korean scientist, Bae et all conducted a study in 2019-2020, in which they examined a non-macrolide + steroid combinatorial regimen on macrolide-resistant Mycoplasma pneumoniae patients. In almost 158 patients, they achieved a healthy response with this combination regimen. So, studies should be conducted on different concomitant therapies that are not resistant up till now.
CONCLUSION:
Pediatrics, along with other populations like geriatrics, pregnant ladies, and lactating mothers, are considered a sensitive or high-risk population. But unlike all the other populations, they possess comparatively sensitive, highly permeable skin & immature organs. So, they need extra care. Despite all of the care given to them, they may be prone to bacterial infections. The antibiotics prescribed to them in order to combat those infections are becoming resistant day by day. Various studies conducted on antimicrobial resistance stewardship programs recommended that preventing the overuse & misuse of antibiotics can somehow decrease the emerging resistance of these antibiotics. Moreover, targeted therapies must be considered by accurately diagnosing & prescribing patterns. The usage of other combined therapies is also an emerging trend found in modern studies to combat the antimicrobial resistance issue in the pediatric population.
I don’t want to say to my children that I didn’t do my best to protect them & their children from
AMR.
FAQS
Q1: How do antibiotics treat bacterial infections?
Ans: Antibiotics either kill the bacteria (bactericidal) or prevent the growth of the bacteria by inhibiting the growth of protein in those bacteria (bacteriostatic), hence bacteria would not be able to grow or cause the infection in organisms.
Q2: What if a child gets a resistant infection?
Ans: If a child gets a resistant infection, the healthcare guardian of the patient must switch to the IV antibiotics or switch to the other group of antibiotics in order to mitigate the child’s infection.
Q3: What are the resistant bacteria commonly called?
Ans: The resistant bacteria may commonly be called SUPERBUGS. It means they have become resistant to many antibiotics.
Q4: Can antibiotic resistance be a cause of death?
Ans: Yes, antibiotic resistance can cause deaths. Almost 35000 deaths per year are caused by antibiotic resistance in the United States of America.
Q5: What is the antibiotic stewardship program?
Ans: Antibiotic stewardship is the process of improving the use of antibiotics and the treatment of bacterial infections effectively. This process also involves eradicating overuse & misuse of antibiotics.
Q6: How can one prevent their children from bacterial infections non-pharmacologically?
Ans: By observing the following routine, one can prevent their children from those bacterial infections that are transmitted by hand:
- Sanitizing hands before/ after eating or playful activity.
- Consuming safe food.
- Proper immunization.
- Use of a mask.
References:
[1] P. J. Gill, T. Thavam, M. R. Anwar, J. Zhu, T. To, and S. Mahant, “Pediatric Clinical Classification System for use in Canadian inpatient settings,” PLoS ONE, vol. 17, no. 8, August. 2022. doi: 10.1371/journal.pone.0273580.
[2] C. Wattal and N. Goel, “Pediatric Blood Cultures and Antibiotic Resistance: An Overview,” Indian J. Pediatr., vol. 87, no. 2, pp. 125–131, 2020, doi: 10.1007/s12098-019-03123-y.
[3] C. Vicentini and C. M. Zotti, “Editorial for the Special Issue ‘Antibiotic Prescribing and Antimicrobial Resistance Patterns in Pediatric Patients,’” Antibiotics, vol. 12, no. 9, pp. 10–12, 2023, doi: 10.3390/antibiotics12091390.






