INTRODUCTION:
Parkinson’s disease is a progressive neurodegenerative disorder that affects approximately 1% of individuals over the age of 60. It ranks second as the most common neurodegenerative disorder. Therefore, it is crucial to understand and raise awareness about the clinical features, pathophysiology, and management of Parkinson’s disease.
ETIOLOGY:
Approximately 80% of Parkinson’s disease cases are idiopathic. However, it also results from a combination of genetic and environmental factors.
TYPES OF PARKINSON’S DISEASE:
- Idiopathic Parkinson’s disease: In most cases, the cause of Parkinson’s disease remains unknown.
- Environmental toxins: Methyl-phenyl-tetrahydropyridine (MPTP) has been identified as a primary cause of Parkinson’s disease in young drug users.
- Medications: Antiemetic and antipsychotic drugs, such as metoclopramide and prochlorperazine, can induce Parkinson-like symptoms.
- Viral infections: Certain viral infections, including encephalitis and neurosyphilis, can cause parkinsonism.
- Genetic mutations: In a few cases, genetic mutations can lead to Parkinson’s disease. Mutations in genes like LRRK2, PARK7, and SNCA have been linked to Parkinson’s.
PATHOPHYSIOLOGY:
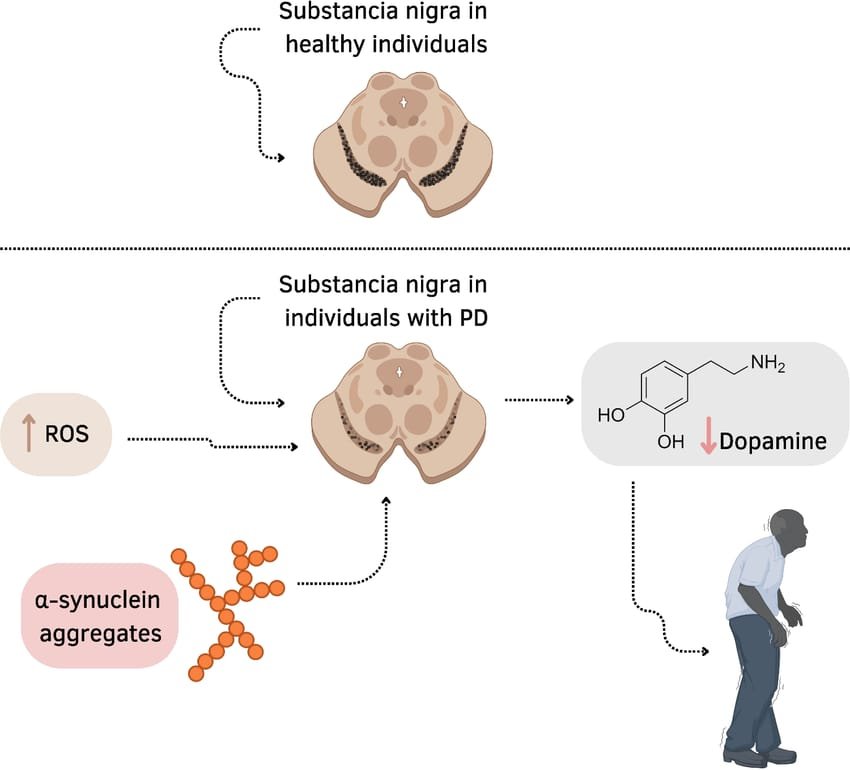
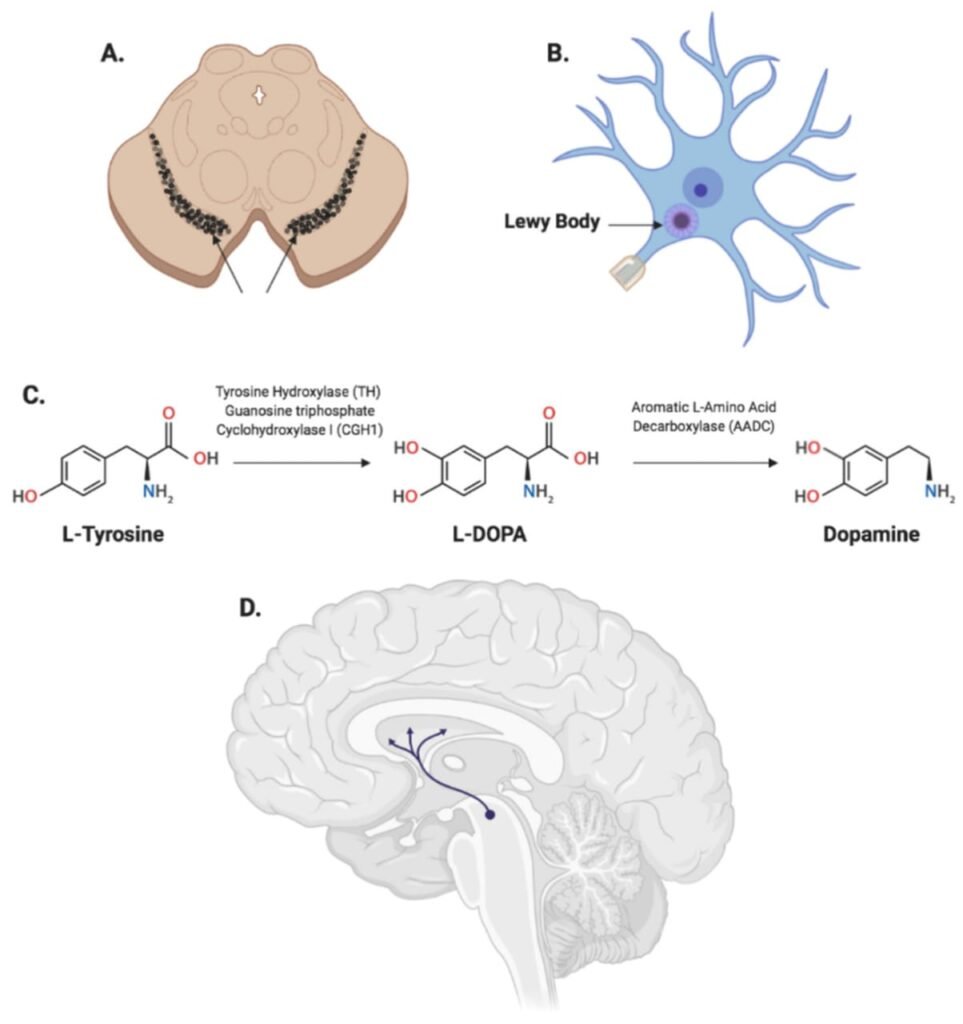
The underlying pathology of Parkinson’s disease involves the loss of dopaminergic neurons in the substantia nigra. Substantia nigra is the region of the brain responsible for producing dopamine; a neurotransmitter accountable for initiating motor movements. This ultimately leads to dopamine deficiency in the basal ganglia. As dopamine levels decline, patients experience motor symptoms such as tremors and rigidity.
Other pathological hallmarks include the presence of α-synuclein and other protein inclusions in nigral cells (Lewy bodies), which disrupt cellular processes and contribute to disease progression.
CLINICAL FEATURES:
The chief clinical features of Parkinson’s disease include a diverse range of motor and non-motor symptoms; varying from patient to patient:
Motor Symptoms:
- Bradykinesia: Difficulty in initiating movement
- Rigidity of the skeletal muscles with associated increased tone
- Stooped posture
- Tremors
- Micrographia: Small handwriting
Non-Motor Symptoms:
- Depression and Anxiety: Mental health issues become more prominent as the disease progresses and can precede motor symptoms.
- Cognitive Impairments: Including dementia.
- Autonomic Dysfunction: Such as constipation, bladder problems
- Amnesia: Anterograde and retrograde
DIAGNOSIS:
Diagnosing Parkinson’s Disease can be challenging, as symptoms may resemble those of other conditions and no definitive tests exist. Key diagnostic tools include:
- Medical History: Evaluating the patient’s medical history, including illnesses, medications, and injuries, is crucial.
- Physical Examination: A clinical evaluation of the patient’s motor symptoms, reflexes, and overall physical condition.
- Imaging Tests: CT scans or MRI scans help rule out other conditions that may cause Parkinson-like symptoms.
- DaTSCAN: A specialized imaging technique that evaluates dopamine levels in the brain, helping confirm Parkinson’s disease diagnosis.
TREATMENT:
Parkinson’s disease is a neurodegenerative disorder and is uncurable. However, drug therapy is clinically effective in delaying the progression of Parkinson’s disease and in providing symptomatic relief.
- Levodopa:
Levodopa, a dopamine precursor, remains the gold-standard treatment for symptomatic relief of Parkinson’s disease. However, its efficacy is limited by peripheral decarboxylation, where 90% of the orally administered drug is converted to dopamine outside the brain, causing unwanted peripheral effects.
To overcome this, Levodopa is co-administered with Carbidopa, a dopa decarboxylase inhibitor (DDI). Carbidopa inhibits peripheral conversion of Levodopa to dopamine, increasing the amount of Levodopa that reaches its target site in the brain.
Levodopa effectively alleviates symptoms of akinesia and rigidity, but its effect on tremors is less satisfactory. Prolonged use of Levodopa can lead to motor fluctuations, including “on-off” phenomena and Levodopa-induced dyskinesia (LID).
- Dopamine Receptor Agonists:
There are two classes of dopamine agonists:
- Ergot drived: Bromocriptine, Pergolide
- Non-Ergot derived: Ropinirole, Rotigotine
These agents work at the dopamine receptors to delay motor complications. Currently, these agents are not recommended because of more adverse effects (including nausea, vomiting, and hallucinations) and are more expensive.
- MAOI-B inhibitors:
Monoamine oxidase type B is an enzyme that is responsible for the breakdown of excess dopamine in the synapse and so, the MAO-B Inhibitors are introduced to prevent dopamine metabolism in the synapse. The drugs included in this class include: selegiline and rasagiline.
- COMT Inhibitors:
Catechol-O-methyltransferase (COMT) is an enzyme, along with dopa decarboxylase, responsible for the peripheral breakdown of Levodopa. To counteract this, COMT inhibitors such as entacapone and tolcapone are used to reduce the peripheral effects of Levodopa.
These inhibitors are available as single tablets or in combination with Levodopa. Tolcapone is more potent than entacapone but is less preferred due to rare yet serious hepatotoxicity.
- Amantadine:
Amantadine, primarily an antiviral drug, has also shown efficacy in managing Parkinson’s disease. It produces mild, typically short-lived effects on bradykinesia. However, due to its adverse effects, including peripheral edema, delirium, and anticholinergic effects, Amantadine is rarely used. It is typically reserved for patients who cannot tolerate other medications.
- Anticholinergic Drugs:
Prior to the introduction of Levodopa, Anticholinergic Drugs were considered as the primary treatment for Parkinson’s Disease. Currently, their use is limited because of their reduced efficacy and serious adverse effects, such as dry mouth, blurred vision, constipation, urinary retention, delirium, and hallucinosis, as well as long-term concerns regarding cognitive impairment.
- Surgical Approach:
In advanced Parkinson’s disease cases, a surgical approach may be considered, including Deep Brain Stimulation (DBS). DBS is a surgical procedure involving the implantation of an electrode in the brain to stimulate dopamine production. It is typically reserved for patients experiencing motor fluctuations and tremors that are unresponsive to pharmacological treatment.
- Physical Therapy:
Physical therapy is generally employed in patients with Parkinson’s disease to reduce the rigidity of the skeletal muscles and to correct their abnormal posture. Regular exercise routines and physiotherapy can help improve mobility and overall motor functions.
CONCLUSION:
Parkinson’s disease is a complex neurodegenerative disorder that affects millions of people worldwide. Clinical features such as tremors, bradykinesia, and postural instability can significantly impact an individual’s quality of life. Parkinson’s disease requires a comprehensive treatment approach. As there is no cure, various treatment options can help elevate the symptoms, slow disease progression, and improve the overall quality of life. By understanding the diagnosis, treatment, and management of Parkinson’s disease, individuals can take control of their condition and live a fulfilling life.
QUESTIONS:
- What is the primary neurotransmitter affected in Parkinson’s disease?
Answer: Dopamine.
- Enlist the common non-motor symptoms of Parkinson’s disease?
Answer: Depression, Anxiety, Fatigue, Sleep Disturbances, and Cognitive Impairment.
- Which of the following pathological features is most characteristic of Parkinson’s disease?
- Accumulation of Lewy bodies in dopaminergic neurons
- Increased levels of beta-amyloid plaques in the brain
- Cortical atrophy and loss of pyramidal cells
- Shrinkage of the thalamus and basal ganglia
Answer: A) Accumulation of Lewy bodies in dopaminergic neurons
- A 60-year-old woman with Parkinson’s disease is experiencing frequent “on-off” fluctuations despite oral levodopa therapy. Which of the following management options is most appropriate for these motor fluctuations?
- Add a COMT inhibitor to her current regimen
- Start a monoamine oxidase-B (MAO-B) inhibitor
- Start transdermal dopamine patches
- Introduce a serotonin-norepinephrine reuptake inhibitor (SNRI)
Answer: A) Add a COMT inhibitor to her current regimen
- A 70-year-old man presents with a 2-year history of gradually worsening tremors in his right hand, bradykinesia, and muscle rigidity. He has difficulty initiating movements and has noticed his handwriting has become smaller and more difficult to read (micrographia). He walks with a shuffling gait and has trouble maintaining balance. On examination, he has resting tremors, and a mask-like facial expression.
What is the most likely diagnosis, and what is the first-line pharmacological treatment?- Essential tremor; Beta-blockers
- Parkinson’s Disease; Levodopa/carbidopa
- Multiple sclerosis; Interferon therapy
- Alzheimer’s disease; Cholinesterase inhibitors
Answer: B) Parkinson’s Disease; Levodopa/carbidopa





