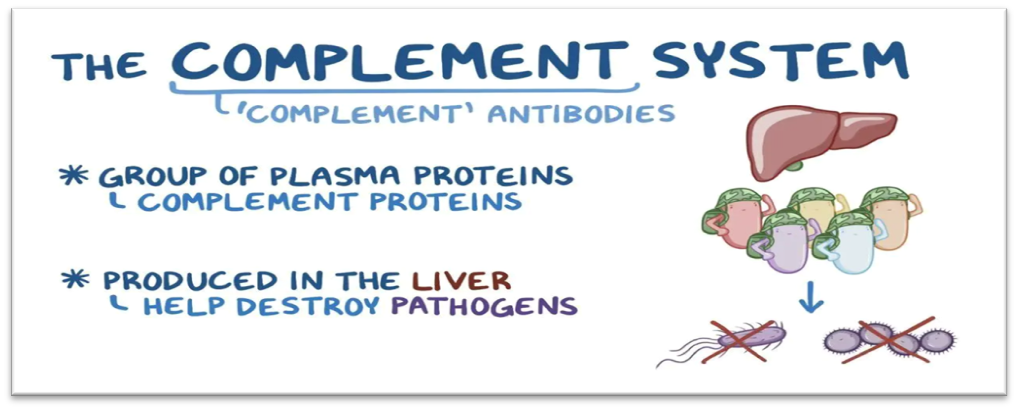
The term complement refers to the ability of these proteins to assist, or complement, the activity of antibodies in destroying (lysing) cells, including microbes. The complement system is made up of a large number of plasma proteins which are heat labile that react with one another to augment or complement the immune response and inflammatory responses that help to fight infection. The Complement system is the major effector of a cellular and humoral branch of the immune system.
History
In 1890s, Jules Bordet at the Pasteur institute in Paris demonstrated that the guinea pig anti-serum to the bacterium Vibrio cholera caused lysis of bacteria and that heating the antiserum destroyed its bacteriolytic activity. However, the ability to lyse bacteria was restored to the heated serum by adding fresh serum which contained no antibodies. Eventually, Paul Ehrlich coined the term Complement.
Functions of Complement
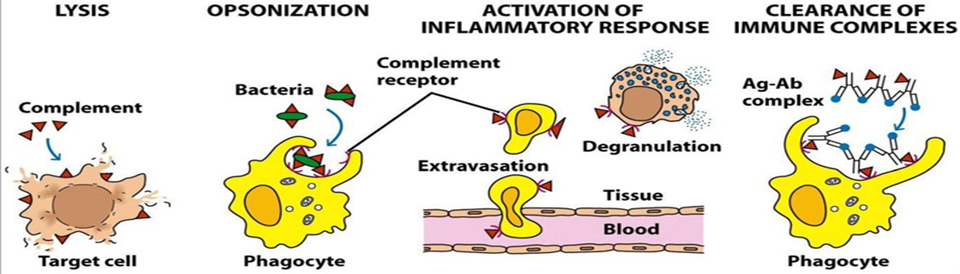
- Lysis of cells, bacteria, and viruses.
- Opsonization which promotes the phagocytosis of particulate antigens.
- Binding to the specific complement receptors on cells of the immune system which triggers specific cell functions, inflammation and secretion of immunoregulatory molecules.
- Immune clearance which removes immune complexes from the circulation and deposits them in the spleen and liver.
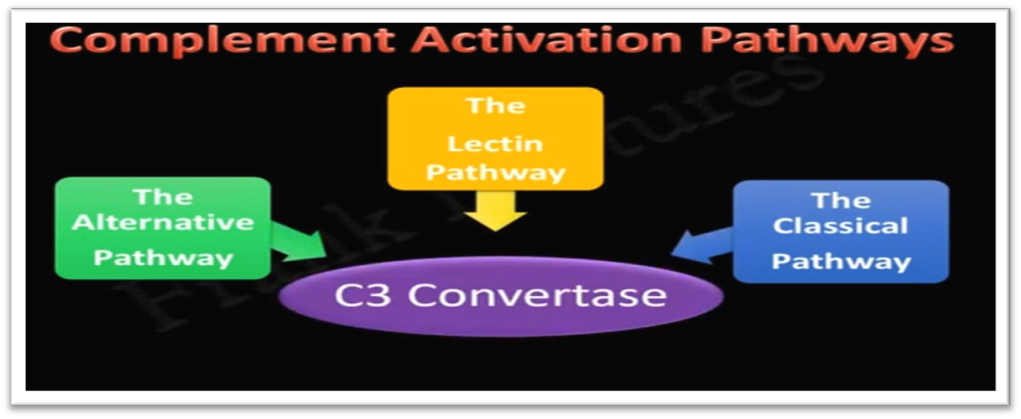
Complement Pathways
There are three major pathways of complement activation: the alternative and lectin pathways are initiated by microbes in the absence of antibody, and the classical pathway is initiated by certain isotypes of antibodies attached to antigens. The early steps, culminating in formation of C5b, can occur by all the three pathways. The final steps that lead to a membrane attack are the same in all pathways.
Biological Consequences of Complement Activation
Complement serves as an important mediator of the humoral response by amplifying the response and converting it into an effective defense mechanism to destroy invading microorganisms. The MAC mediates cell lysis, while other complement components or split products participate in the inflammatory response, opsonization of antigen, viral neutralization, and clearance of immune complexes. Many of the biological activities of the complement system depend on the binding of complement fragments to complement receptors, which are expressed by various cells. In addition, some complement receptors play an important role in regulating complement activity by binding biologically active complement components and degrading them into inactive products.
1. The Membrane-Attack Complex can lyse a broad spectrum of cells
The membrane-attack complex formed by complement activation can lyse gram negative bacteria, parasites, viruses, erythrocytes, and nucleated cells.
2. Cleavage products of complement components mediate inflammation
The smaller fragments resulting from complement cleavage, C3a, C4a, and C5a, called anaphylatoxins, bind to receptors on mast cells and blood basophils and induce degranulation, with release of histamine and other pharmacologically active mediators. The anaphylatoxins also induce smooth-muscle contraction and increased vascular permeability.
3. C3b and C4b binding facilitates opsonization
C3b is the major opsonin of the complement system, although C4b and C3b also have opsonizing activity. The amplification that occurs with C3 activation results in a coating of C3b on immune complexes and particulate antigens.
4. The complement system neutralizes viral infectivity
Large viral aggregates reduce the net number of infectious viral particles. Antibody bind to viral particle creates a thick protein coating that neutralizes viral infectivity by blocking attachment to susceptible host cells.
5. The complement system clears immune complexes from circulation
Erythrocytes play an important role in binding C3b-coated immune complexes and carrying these complexes to the liver and spleen. In these organs, immune complexes are stripped from the red blood cells and are phagocytosed, thereby preventing their deposition in tissues.
Complement Mediated Diseases
- Deficiency of complement especially C5–C8, greatly enhances susceptibility to Neisseria bacteremia and other infections. A deficiency of C3 leads to severe, recurrent pyogenic and respiratory tract infections.
- When type A blood is given by mistake to a person who has type B blood, antibody to the A antibody in the recipient binds to A antigen on the donor red cells, complement is activated, and large amounts of anaphylatoxins and membrane attack complexes are generated. The anaphylatoxins cause shock, and the membrane attack complexes cause red-cell hemolysis.
- Acute glomerulonephritis and systemic lupus erythematosus
Immune complexes bind complement, and thus complement levels are low in immune complex diseases. The binding (activating) complement attracts polymorphonuclear leukocytes, which release enzymes that damage tissue.
- Increase in complement-mediated hemolysis
Clinically, this appears as the disorder paroxysmal nocturnal hemoglobinuria (PNH) which manifests as increased fragility of erythrocytes, leading to chronic hemolytic anemia, pancytopenia (loss of blood cells of all types) and venous thrombosis (formation of blood clots).
- Patients with severe liver disease, e.g., alcoholic cirrhosis or chronic hepatitis B, who have lost significant liver function and therefore cannot synthesize sufficient complement proteins, are predisposed to infections caused by pyogenic bacteria.
Conclusion
Overall, the complement system consists of a large number of plasma proteins which complement the immune response and inflammatory responses that help to fight infection. However, there are three pathways of complement activation, the alternative and lectin pathways are initiated by microbes in the absence of antibody, and the classical pathway is initiated by certain isotypes of antibodies attached to antigens. While deficiencies in complement components can lead to diseases, infections, autoimmune diseases and renal diseases.
FREQUENTLY ASKED QUESTIONS (FAQs)
- What are the functions of the complement system?
The complement systems functions include Protection, Inflammation, Removal and Regulation.
- What can happen if the complement system is imbalanced?
An imbalance between complement activation and regulation can lead to disease and injury.
- What diseases can be associated with complement deficiencies?
Deficiencies in complement components can lead to diseases such as infections, autoimmune diseases and renal diseases.
- How the complement system activated?
The complement system can be activated by the classical or alternative or lectin pathway.
- What is the end goal of complement system?
The end result of this complement activation is the stimulation of phagocytes to clear foreign and damaged material, inflammation and activation of the cell killing membrane attack complex.






