Button batteries are also known as disc shaped or coin like shaped that is commonly used in household devices such as calculators, motor toys, and watches. Button batteries are not edible but in children its ingestion may lead to life threatening conditions.
Incidence: Foreign body ingestion is most common in children aged 6 months to 3 years. While 30% of cases may be asymptomatic, any suspicion of ingestion warrants investigation.
A thorough investigation of over 8000 patients revealed over 1600 adult ingestions from 1990 to 2008, despite the fact that the majority of ingestions occur in the juvenile group. One Therefore, both pediatric and adult health care practitioners might benefit from the present overview of this topic. In order to avoid serious consequences that could come from prolonged exposure, the clinician must promptly identify and treat BB aspiration, ingestion, or insertion. The most recent additions to the treatment guidelines, such as mitigation and neutralization techniques based on the most recent data, should also be known by providers. Airway obstruction problems and nasal septalor tympanic membrane perforations are among the morbidities that can result from the aspiration of smaller BBs into the tracheobronchial tree, nasal cavity, or ear canal.
Mechanism of Toxicity
- It creates an electric current that may disrupts the integrity of blood vessels in the gut.
- It put pressure on the sensitive tissues and cause inflammation.
- It can leak certain chemicals from anode or cathode that cause burns in throat, the voice box damages and bleeding may occurs.
WHAT MAKES A BATTERY TOXIC?
Button batteries are composed of several components that may lead to their toxicity including:
- Anode – Zinc oxide is used normally that may release zinc ions and corrode the tissues.
- The recommended daily adult zinc intake is 15 mg. Symptoms usually do not appear until ingestions exceed 1 to 2 g of zinc.
- Smaller batteries contains approximately 5g of Zinc oxide while larger contains 10g of it.
- Cathode – Commonly made of manganese dioxide (MnO₂), silver oxide (Ag₂O), or carbon monofluoride (CFₓ), these are usually nontoxic in nature.
- Electrolyte- It contains the alkaline solutions of NaOH (Sodium hydroxide) and KOH (Potassium hydroxide) that may leaks into tissues and lead to toxicity.
- Corrosives exposures to the internal lining of the body.

Signs and Symptoms:
Within 2 hours of ingestion button battery cause serious esophageal injuries. The most common symptoms after button battery ingestion are vomiting, dysphagia, fever and coughing.
The signs and symptoms are broadly categorized into two main types:
- EARLY SYMPTOMS – It includes sore throat, trouble in swallowing and coughing.
- LATE SYMPTOMS – It consists of difficulty in breathing, abdominal pain, chest pain, vomiting and shock.
Serious complications may include all these:
- Esophageal-tracheal fistula
- Esophageal perforation
- Esophageal stenosis
- Vocal cord paralysis
- Mediastinitis
- Pneumothorax
- Aspiration pneumonia,
- Empyema
- Lung abscess
- Spondylodiscitis
- Esophageal-aortal fistula
- Respiratory and circulatory failure
DIAGNOSTICS:
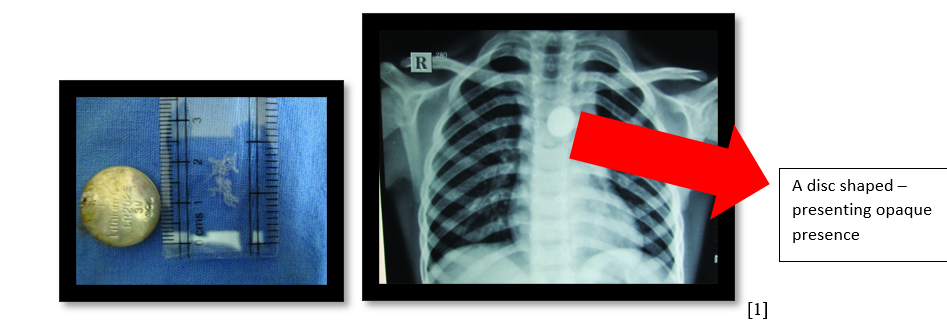
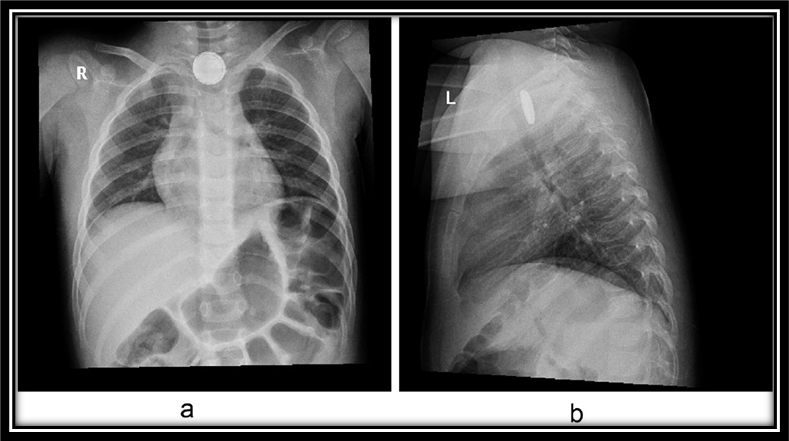
- Radiographic Imaging– It is the most appropriate radiological examination by which button batteries are identified .Button batteries appear as a circular, radiopaque objects.
- Both anteroposterior and lateral views are usually taken to evaluate exact location of button battery.
- CT scan – It is not usually used but can be used for complex cases to determine the esophageal complications (perforations, fistula or mediastinitis).
- Endoscopy -Used for the removal of button battery.
MANAGEMENT AND TREATMENT GUIDELINES:
Pre-Removal
Administer 10 mL (two teaspoons) of honey every 10 minutes until the patient reaches the hospital. Do not give honey to children under one year of age at home.
Provide 10 mL (two teaspoons) of Sucralfate (Carafate) every 10 minutes until the button battery (BB) can be removed. This can begin even before X-ray confirmation if ingestion is strongly suspected or observed in hospital settings.
According to the National Capital Poison Center (NCPC), up to six doses are recommended in prehospital care and up to three additional doses in the clinical setting. If there are delays, such as extended transport to another facility, clinical judgment should guide whether further doses are needed.These measures are only temporary and do not replace the need for urgent removal of the battery from the esophagus.
Removal
The removal of an esophageal BB is a medical emergency and must be addressed immediately, regardless of the patient’s fasting (NPO) status.
- Rapid sequence induction is required.
- Utilize an endoscopic method with direct visualization, either with flexible or rigid esophagoscopy.
- Assess for laryngotracheal injury or the development of a tracheoesophageal fistula using direct laryngoscopy and bronchoscopy. This is particularly important if the BB’s negative pole is facing forward (anterior step-off).
- Be prepared for complications such as esophageal perforation, tracheoesophageal fistula, vocal cord issues (paresis or paralysis), or the battery’s proximity to major blood vessels (e.g., an arterial fistula).
- If there is no evidence of perforation, perform endoscopic irrigation of the injury site using 50–150 mL of 0.25% sterile acetic acid while suctioning the fluid simultaneously.
- In cases of suspected perforation or significant circumferential damage, consider inserting a nasogastric tube during the procedure.
Post-Removal
Tissue damage can continue to worsen even after the BB has been removed.
- Conduct an esophagram to rule out perforation before resuming oral intake. If there is significant damage, use imaging techniques such as MRI or CTA to assess the proximity of the injury to major blood vessels (e.g., the aorta).
- Monitoring: Watch for delayed complications, which can include esophageal perforation, tracheoesophageal or aortoesophageal fistulas, vocal cord dysfunction (paresis or paralysis), mediastinitis, spondylodiscitis, or strictures in the esophagus. These issues may emerge days or even weeks later.
Case # 01 A case is reported in India in between 2013-2014.
A young 8 years old mentally subnormal male child arrived in an emergency room to a hospital with a chief complain of pain in abdomen, the pain is started in periumbilical region and it radiated to back. There was no history of vomiting and no history of fever. Parents are complaining of some abnormal behavior such as unable to talk properly, unable to swallow the food and restlessness.
Physical and systemic examination is normal, CBC (Complete Blood Count) is unremarkable but a chest X-ray showed the presence of foreign body at T4 vertebral level.
Rigid esophagoscopy revealed a button battery lodged in the esophagus, covered with sloughed mucosal tissue. The foreign body was 3V Lithium button battery. The battery then removed and ulceration is healed by providing the treatment of Pantoprazole and Sucralfate.
After 2 months of follow up the child showed no complications and recovery was remarkable.
CASE # 02
King Abdul Aziz Medical City (KAMC), Jeddah, Saudi Arabia
After two days continuous drooling, a healthy 2-year-old girl’s mother noticed and brought her to our emergency room (ED). The young child had repeatedly been playing with disc batteries, according to the mother. The girl was given antibiotics after being diagnosed with pharyngitis at a clinic earlier, but the next day, her symptoms, which included fever and vomiting, got worse.
Her parents took her to the hospital when a chest X-ray showed a disc battery stuck in her upper esophagus.
The child had a set of symptoms included:
- high fever (40°C)
- shortness of breath
- A fast heartbeat (150 beats per minute)
- A respiratory rate of 34 breaths per minute when she went to the emergency department. The disc’s existence was verified by the chest X-ray. Batteries were present in the esophagus without any obvious signs of pneumothorax, pneumonia, or other medical conditions.
To remove the disk battery, the child had an emergency esophoscopy. Doctors observed a battery-induced burn in the esophagus during the treatment, but they didn’t observe perforations.
Treatment: Following the treatment, the kid received intravenous fluids, antibiotics (amoxicillin/clavulanic acid), and a medicine to lower stomach acid (H2 blocker) while being monitored in the pediatric intensive care unit (PICU).
No esophageal strictures or leaks were discovered during a follow-up swallow test using contrast. The child’s diet was progressively transitioned from clear fluids to soft foods, and she was sent home with instructions to come back if she experienced any symptoms, such as fever, drooling, or trouble swallowing.
One month later, the child was eating normally, and repeat imaging showed no esophageal damage. Follow-ups at three and six months confirmed her recovery, and all medications were discontinued.
CASE # 03
Pediatric department of Dakar Principal Hospital-Senegal (West Africa)
A coughing 13-month-old baby with a gastrostomy feeding tube had been admitted in. She’d swallowed a big button battery from a portable radio by accident two weeks prior. When the mother noted vomiting, profuse drooling, and an open battery compartment, she suspected the battery. She tried using milk and water to make herself throw up, but the battery did not come out.
Two hours after the event, the child was taken to the hospital. A gastrostomy feeding tube had to be inserted after an attempt to remove the battery 36 hours later with a rigid endoscope caused an esophageal perforation.
Treatment-The infant was admitted with signs of bronchial congestion, insignificant malnutrition, and dehydration. Despite a normal chest X-ray, an esotracheal fistula—an irregular attachment between the esophagus and trachea—was discovered during a barium swallow test (BST). A 10 mm fistula close to the upper esophagus was confirmed by endoscopy.
This was addressed by removing the gastrostomy tube and performing a feeding jejunostomy. By trimming the fistula’s margins and using clips to seal it, the doctors attempted to close it endoscopically. On day 15, however, a follow-up BST revealed that the fistula was only half closed, and the patient was still experiencing issues, such as a bronchogram.
Unfortunately, persistent problems led to the child’s death from inhalation pneumonitis.
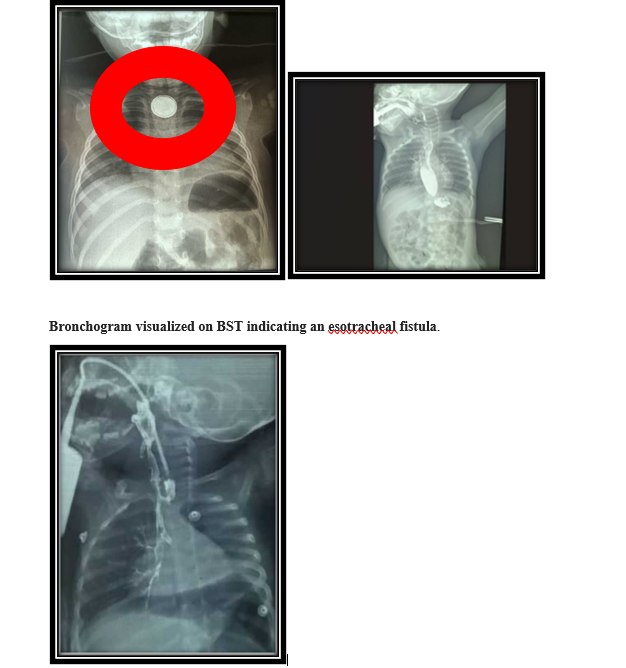
Right-sided bronchogram on follow-up BST suggests a partial closure of the esotracheal fistula.
A CASE SCENARIO – REAL CASE OF LAHORE
Department of Pediatric Gastroenterology, Hepato-logy, Children’s Hospital and University of Child Health Sciences, Lahore Pakistan, from July 2021.
My aunt’s daughter of about 1 year old was playing with her toys which included automatic battery based toys, the batteries were uncovered, after three days her daughter refused to eat anything because there was a problem to swallow it the child was presented to emergency department of hospital in Lahore with a chief complain of Dysphagia and coughing.
Physical examination and systemic examination was normal then radiological reports were recommended. Upon the arrival of chest x ray it was found out that there was a disc based shape in the chest X-ray and upon revealing the history her mother told about them a button batteries of her toys.
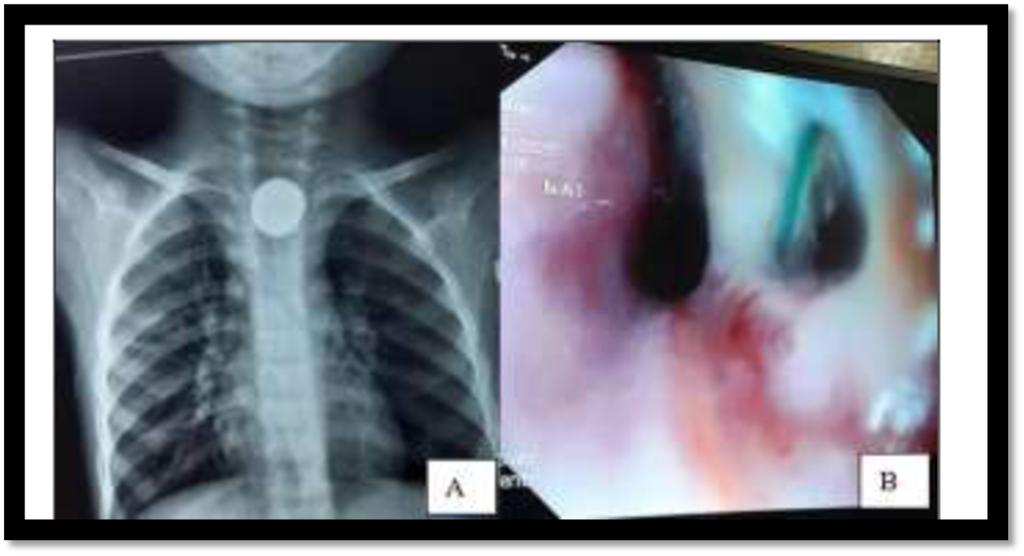
Upon endoscopy the battery was removed but there was numerous perforations in mucosa. After endoscopy she sent to the esophagus repair but unfortunately she died due to sepsis.
References:
1. Kalyanshettar, S., S. Patil, and G. Upadhye, Button battery ingestion-case report and review. J Clin Diagn Res, 2014. 8(9): p. Pd01-2.
2. Sindi, E., et al., Disc battery ingestion; a single event with different outcomes. International Journal of Pediatrics and Adolescent Medicine, 2017. 4(2): p. 87-90.
3. Fall, M., Nakoulima, A.D., Fall, K., Goumba, A.I., Seck, M.A., Niang, T., Mboup, M., Mbacké, M.D., Diallo, I. and Seye, M.N. (2024) Button Cell Ingestion in Infants: A Report of Five Cases. Journal of Biosciences and Medicines, 12, 199-209




