A toxidrome, or toxic syndrome, refers to a collection of signs, symptoms, and characteristics that are consistently linked to certain classes of toxins or poisons. Recognizing a toxidrome is crucial in toxicology and emergency medicine, as it can aid in determining the type of poisoning or overdose and guide the proper treatment.
So, a cholinergic toxidrome occurs when the nervous system is overactive because of an accumulation of acetylcholine, resulting from an excessive stimulation of cholinergic receptors. The most frequent cause of this illness is exposure to cholinesterase inhibitors, which include carbamates, organophosphates, and cholinergic agonists. Therefore, early detection and treatment of this life-threatening illness are important for better patient outcomes.
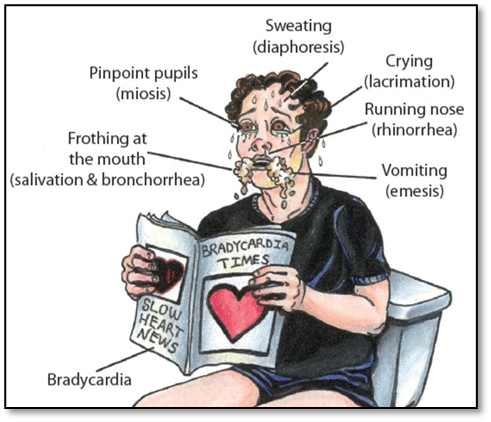
Moving towards pathogenesis. Cholinergic toxidrome is caused by the suppression of acetyl cholinesterase (AChE), an enzyme that degrades acetylcholine (ACh). Elevated ACh levels cause overstimulation of muscarinic and nicotinic receptors, which can be identified by characteristic clinical features. Cholinergic toxidrome can present with symptoms that are categorized into muscarinic, nicotinic, and central effects. The well-known mnemonic DUMBELS explains the symptoms associated with the muscarinic effects:
- D: Diarrhea
- U: Urination
- M: Miosis
- B: bronchospasm, bradycardia
- E: Emesis
- L: Lacrimation
- S: Salivation, sweating
Nicotinic Symptoms include: muscle fasciculation’s, weakness or paralysis, hypertension and tachycardia, while Central Nervous System Symptoms involve: anxiety, confusion, seizures or coma.
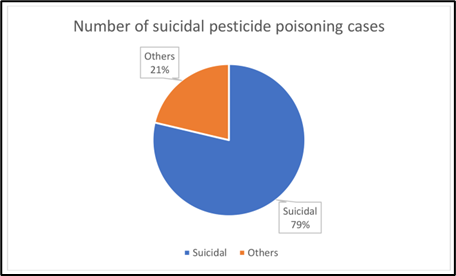
Cholinergic poisoning, mainly caused by exposure to organophosphate (OP) pesticides, is a major public health concern in Pakistan. About 30-50% of poisoning incidents in tertiary care hospitals are linked to organophosphate poisoning. The death rates vary between 10-30%, influenced by how accessible medical care is and how quickly treatment is provided.
In diagnosing cholinergic toxidrome, healthcare professionals need to exclude other conditions that present with similar symptoms. For example, in cases of opioid overdose, both can lead to constricted pupils; however, but opioids typically cause slow breathing, not excessive secretions. Assessing serum cholinesterase or RBCs acetyl cholinesterase levels is also important, for the reason that their activity decreases in the event of poisoning. Ultimately, precise diagnosis relies on the patient’s history (such as contact with pesticides) and visible symptoms, including constricted pupils, sweating, and an abundance of fluids.
Early recognition and rapid treatment significantly improve outcomes. Treatment involves strong supportive care along with specific therapy for cholinergic toxicity, which includes administering atropine and then using an oxime like pralidoxime if it’s available. It’s also crucial to use decontamination methods and personal protective equipment to stop the patient from absorbing more of the harmful agent and to protect the caregivers from any danger.
– Atropine is used to counteract muscarinic effects and
– Pralidoxime works to reactivate acetyl cholinesterase enzyme.
To conclude our topic, cholinergic toxidrome presents a considerable medical challenge, particularly in agricultural and industrial environments. A thorough understanding of its pathophysiology, along with strict adherence to evidence-based management protocols, is crucial for saving lives and minimizing morbidity.

Some Clinical Pearls for you:
- Early recognition and treatment are essential for survival in cholinergic toxidrome.
- Atropine dosage may vary significantly; focus on clinical endpoints rather than fixed doses.
- Pralidoxime is ineffective for carbamate poisoning but crucial for organophosphate toxicity.
- Continuous monitoring of respiratory function is essential due to the risk of delayed paralysis.
- Always suspect cholinergic toxidrome in patients presenting with the DUMBELS symptoms, particularly after potential exposure to pesticides.
Common FAQs about Cholinergic Toxidrome
- What is cholinergic toxidrome?
Cholinergic toxidrome is a syndrome caused by excessive activation of the parasympathetic nervous system due to increased levels of acetylcholine. It often occurs due to exposure to organophosphate or carbamate pesticides, nerve agents, or certain medications like pilocarpine or acetyl cholinesterase inhibitors.
- What are the main symptoms of cholinergic toxidrome?
Symptoms can be remembered using the acronym SLUDGE-M: Salivation, Lacrimation, Urination, Diarrhea, Gastrointestinal distress, Emesis (vomiting), Miosis (constricted pupils). Other signs include bradycardia, wheezing, sweating, and seizures in severe cases.
- How is cholinergic toxidrome diagnosed?
Diagnosis is primarily clinical, based on symptoms and history of exposure to suspected agents like pesticides or nerve gases. Laboratory tests may include measuring acetyl cholinesterase activity, which is often decreased in cases of organophosphate poisoning.
- What is the treatment for cholinergic toxidrome?
Treatment involves: Atropine: Blocks the effects of excessive acetylcholine on muscarinic receptors. Pralidoxime (2-PAM): Reactivates acetyl cholinesterase and reverses the effects of organophosphates. Supportive care, such as maintaining airway and ventilation, and controlling seizures with benzodiazepines.
- How can cholinergic toxidrome be prevented?
Prevention includes: Safe handling and proper storage of pesticides. Use of personal protective equipment (PPE) during pesticide application. Public education on the risks of organophosphate exposure. Adherence to regulatory guidelines for pesticide usage and disposal.
References:
- https://www.ncbi.nlm.nih.gov/books/NBK482433/#:~:text=Excessive%20accumulation%20of%20acetylcholine%20(ACh,%2C%20diarrhea%2C%20and%20blurry%20vision.
- https://www.sciencedirect.com/topics/nursing-and-health-professions/cholinergic-crisis
- https://www.osmosis.org/answers/sludge-cholinergic-crisis-signs-and-symptoms-acronym
- https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-023-15505-1





