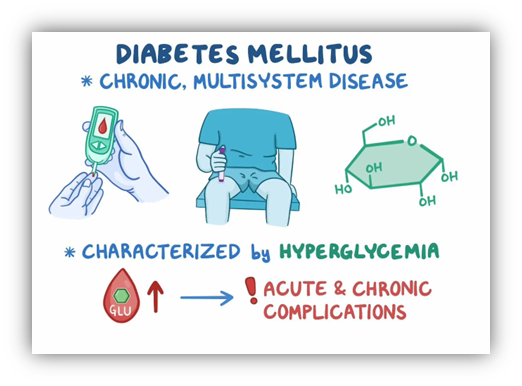
Diabetes is a disease that occurs when your blood glucose, also called blood sugar, is too high. Diabetes is characterized by hyperglycemia due to decreased insulin secretion (from the pancreas), decreased insulin sensitivity (primarily in muscle cells) or both. Chronic hyperglycemia leads to many complications, including organ and nerve damage.
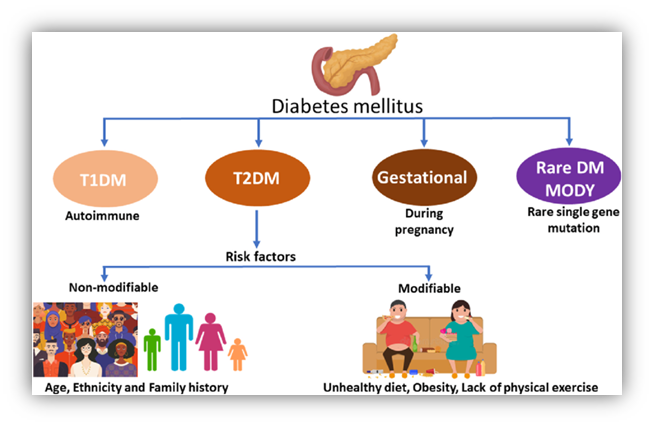
The most common types of diabetes are type 1, type 2, and gestational diabetes.
- Type 1 diabetes accounts for -5% of all cases of diabetes. It is caused by an autoimmune destruction of the beta cells in the pancreas.
- Type 2 diabetes accounts for -95% of cases and is due to both insulin resistance (decreased insulin sensitivity) and insulin deficiency.
- Pre-diabetes means that there is an increased risk of developing diabetes. Following dietary and exercise recommendations reduces the risk of progression from pre-diabetes to diabetes.
- Gestational diabetes is a type of diabetes that develops during pregnancy. Women who develop GDM have an increased risk of developing type 2 diabetes later in life. If the mother has uncontrolled diabetes in pregnancy, the baby can be large (macrosomia), will be at risk for hypoglycemia at birth, and will have a high risk for childhood obesity and type 2 diabetes
- A less common type of diabetes, called monogenic diabetes, is caused by a change in a single gene. Diabetes can also come from having surgery to remove the pancreas, or from damage to the pancreas due to conditions such as cystic fibrosis or pancreatitis.
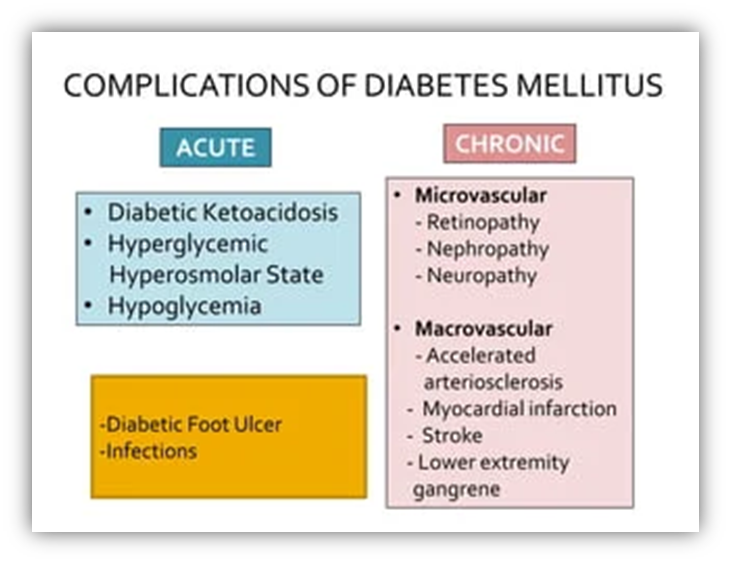
Diabetes, a chronic metabolic disorder, can lead to several acute and chronic complications if not well managed. Uncontrolled diabetes can cause metabolic imbalance leading to acute complications that may require immediate medical attention. Hyperglycemia (high levels of glucose in blood) sets the stage for protein glycation, which in turn may lead to chronic conditions requiring constant monitoring and treatment. Individuals with diabetes may also develop high cholesterol and high blood pressure, which require medical management.
Acute complications are those that arise swiftly and include conditions such as:
- Diabetic ketoacidosis (DKA),
- Hyperglycemic hyperosmolar state (HHS),
- Lactic acidosis (LA), and
- Hypoglycemia.
In contrast, chronic complications progress gradually and are typically divided into two main categories:
- Microvascular complications
- Macrovascular complications
Acute Complications of Diabetes
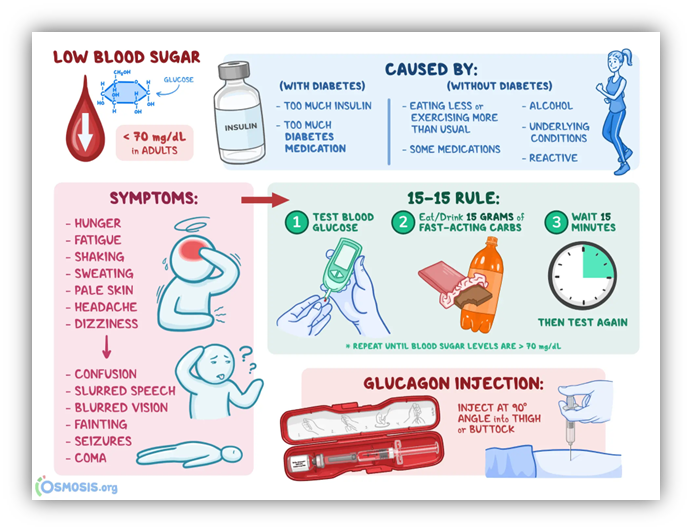
· Hypoglycemia:
Hypoglycemia is defined as a blood glucose <70 mg/dL. The lower the level, the more symptomatic the patient. Hypoglycemic symptoms include dizziness, headache, anxiety, irritability, shakiness, diaphoresis (sweating), hunger, confusion, nausea, lack of coordination, tremors, palpitations or fast heart rate and blurred vision. Seizures, coma and death can occur with severe hypoglycemia. Insulin is the primary cause of drug-induced hypoglycemia. Drugs that make the body secrete more insulin, such as SUs and meglitinides (insulin secretagogues), and pramlintide (which is used with insulin at mealtimes), are also high-risk. All beta-blockers can mask hypoglycemia symptoms of shakiness, palpitations and anxiety (sweating and hunger are not masked). This can prevent prompt recognition of low blood glucose and can result in more severe hypoglycemia.
Glucose is the preferred treatment of hypoglycemia, but any form of carbohydrate that contains glucose will raise blood sugar. Treat hypoglycemia with the following steps, commonly called the “rule of 15”. Glucagon should be prescribed for all patients at significant risk of severe hypoglycemia. Glucagon administration is not limited to healthcare professionals; caregivers and family members should be instructed on its administration. Glucagon 1 mg is given by SC, IM or IV injection. Glucagon must be reconstituted prior to administration.
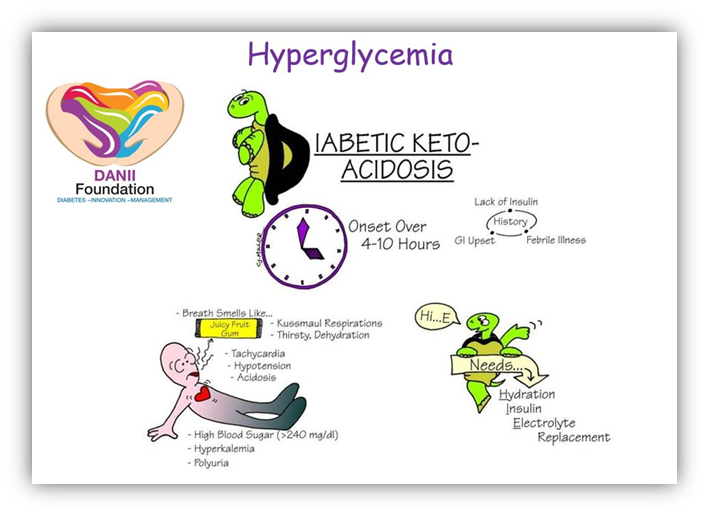
- Diabetic Ketoacidosis (DKA)
Diabetic ketoacidosis (DKA) is a hyperglycemic crisis that most commonly presents in patients with type 1 diabetes, but can present in type 2 diabetes. DKA occurs due to insulin non-compliance, sub-therapeutic insulin dosing, a condition that can cause hyperglycemia (e.g., a stressor, such as infection, MI or trauma), or as the initial presentation in a patient with type 1 diabetes.
Cells begin to utilize fats as an energy source under these circumstances. Hepatic cells generate ketone bodies from fatty acids. In situations where glucose levels are diminished, neuronal cells can metabolize ketone bodies for energy, although they cannot utilize free fatty acids. Elevated levels of ketones may lead to acidic urine and a distinctive fruity odor in breath. If left un-addressed, this condition has the potential to advance to coma, characterized by prolonged unconsciousness, and may ultimately result in death.
Fluid resuscitation and maintenance, insulin therapy, electrolyte replacement, and supportive care are the mainstays of management in diabetic ketoacidosis.
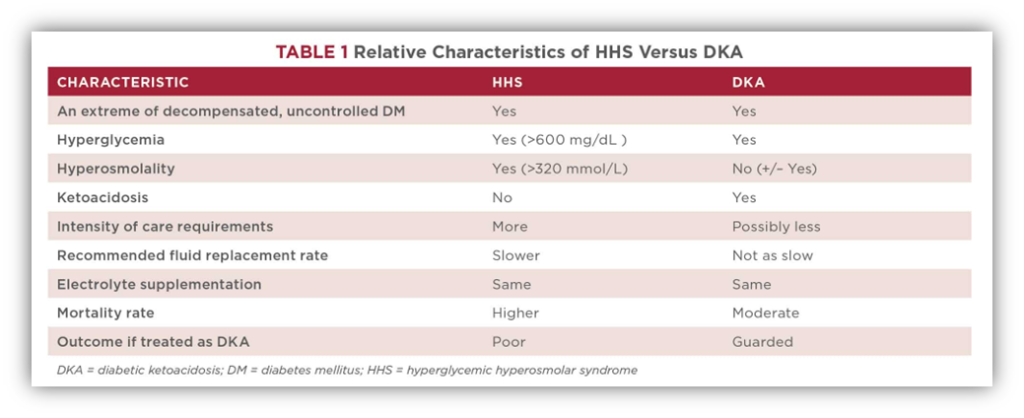
- Hyperosmolar Hyperglycemic State (HSS)
Hyperosmolar hyperglycemic state (HHS) is a hyperglycemic crisis that most often occurs in type 2 diabetes due to some type of severe stress. Serum ketones are negligible or not present because the patient with type 2 diabetes has enough insulin to suppress ketogenesis. The blood glucose is usually much higher at presentation because acidosis is not present and the patient can endure the symptoms longer.
Symptoms include extreme dehydration, hyperglycemia, and altered consciousness. Treatment consists of IV saline, correction of hypokalemia, and IV insulin. Treatment is 0.9% (isotonic) saline solution; 1000 mL is given in the first hour. Smaller boluses (500 mL) can be given if there is risk for exacerbation of heart failure or volume overload.
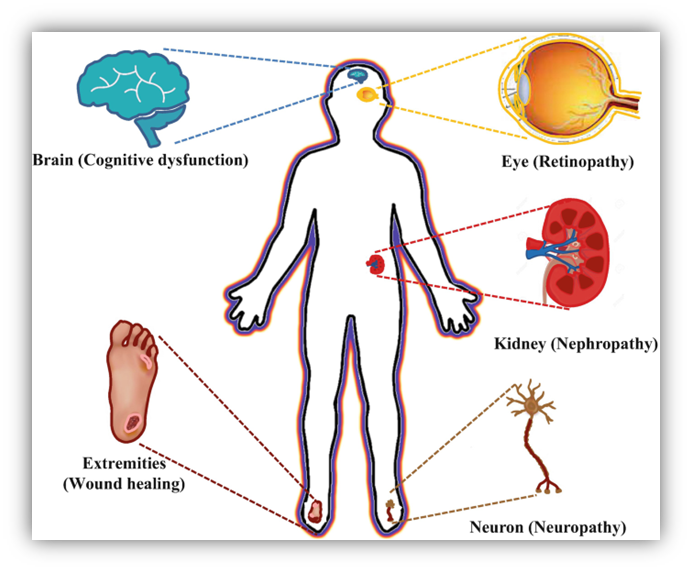
Chronic Complications of Diabetes
- Microvascular Complications:
Microvascular complications include: Kidney disease (Nephropathy), Blindness (retinopathy) and Amputations (the end result of Neuropathy).
Diabetic retinopathy represents the most characteristic and widespread complication of diabetes, serving as a significant contributor to global blindness. Regular comprehensive dilated retinal examinations are essential for the effective management of this condition. Additionally, cataracts (clouding of the lens), glaucoma (elevated intraocular pressure), and varying refractive errors are frequently linked with retinopathy.
Diabetic Nephropathy involves continuous protein leakage in the urine, which causes the kidneys to filter less effectively. This is indicated by higher serum creatinine levels and can progress to advanced kidney disease.
Diabetic Neuropathy is a common complication in many patients, though it is not very specific. It can cause symptoms like foot pain and problems with sweating and movement, which may result in foot ulcers and amputations. Basic foot care practices, such as checking your feet daily, managing calluses, and taking care of your nails, are very important.
Autonomic Neuropathy can lead to issues like erectile dysfunction, constipation, low blood pressure when standing, not noticing low blood sugar, and problems with urine control.
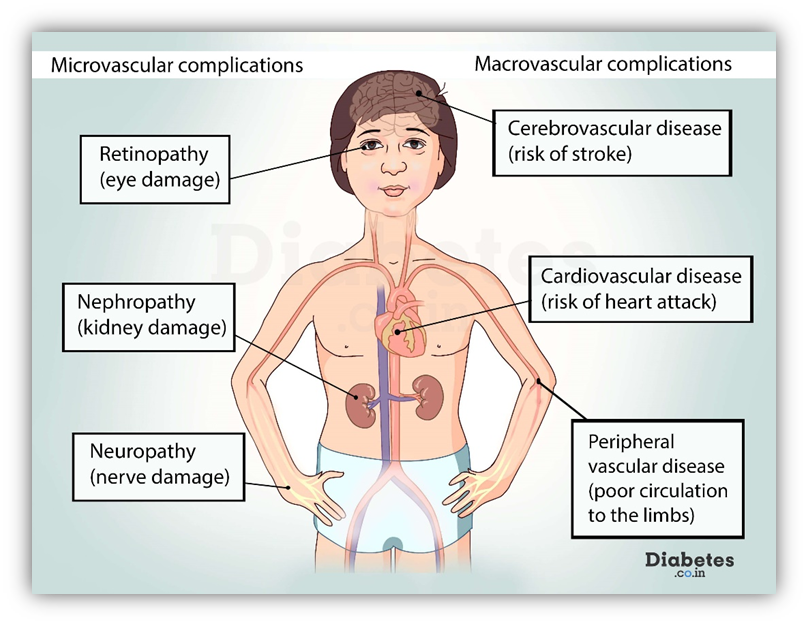
- Macrovascular complications
Macrovascular complications include: coronary artery disease (heart attacks), brain strokes, and peripheral vascular disease. High blood sugar levels are not strongly linked to their severity. Other risk factors, such as high blood pressure, smoking, obesity, and issues with lipids, may be more important in causing these problems.
Coronary heart disease (CHD) is the leading cause of death among people with diabetes. In many places, diabetes is viewed as equivalent to CHD. Managing new diabetes effectively over time has been linked to a lower rate of CHD. However, aggressive treatment for advanced diabetes has produced varied outcomes and is not recommended by specialists. Recently, oral medications such as SGLT2 inhibitors and GLP-1 agonists have gained interest for their heart-protecting benefits.
Strokes are mainly classified into three types: Ischemic (clots blocking blood flow in the vessel), Embolic (clots that break off from another location, like the heart, and block a vessel), and Hemorrhagic (a rupture in the vessel wall causing blood to leak). Common symptoms include trouble speaking, weakness in the arms and legs, and a drooping mouth. The extent of neurological damage varies based on how much blood supply is affected in certain brain areas. In severe cases, complete recovery can take several months.
Peripheral vascular disease (PVD) along with neuropathy is a major reason for non-traumatic amputations of the lower limbs worldwide. Common symptoms include pain in the lower legs not related to joints, rest pain, intermittent claudication (pain in the calves and thighs during activity), and darkening of the toes (gangrene). Diabetic foot ulcers and osteomyelitis, which is a bone infection, are common issues linked to peripheral vascular disease (PVD), leading to long-term health problems.
Skin and joint issues such as limited joint movement, shin spots, frozen shoulder, and carpal tunnel syndrome are also frequent. Additionally, periodontal disease affecting the teeth and gums is common among patients.
Role of Pharmacist in Managing Complications of Diabetes:
Pharmacists are essential in helping manage diabetes and its complications. They do this by educating patients, managing medications, and providing preventive care.
- Teach patients to identify early signs and symptoms of complications such as neuropathy, nephropathy, and retinopathy.
- Offer advice on lifestyle changes, including healthy eating, physical activity, and quitting smoking.
- Make sure patients use anti-hyperglycemic medications, insulin, and other treatments effectively. Work with healthcare teams to adjust medication plans as needed.
- Teach proper use of glucometers and continuous glucose monitors (CGMs). Examine glucose patterns to improve blood sugar management and lower the chances of complications.
- Promote regular checks for both microvascular and macrovascular issues, such as foot exams, eye tests, and kidney function assessments. Look for early warning signs of problems like foot ulcers, high blood pressure, and heart risks.
- Suggest diet plans to help avoid high blood sugar and deal with issues like gastroparesis or dyslipidemia.
- Give advice on what to do in case of low or high blood sugar emergencies.
- Teach the importance of good foot care and choosing the right shoes to stop ulcers and infections. Recommend regular foot checks and visits to podiatrists for patients at risk.
- Organize or take part in diabetes self-management programs (DSMPs) to help patients take control of their health and handle complications.
References:
- https://diabetes.co.in/what-are-the-long-term-complications-of-diabetes/
- https://diabetes.org/about-diabetes/complications
- https://www.endocrine.org/patient-engagement/endocrine-library/diabetes-complications
- https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes
- https://www.who.int/news-room/fact-sheets/detail/diabetes





