Beta-lactam antibiotics have been widely used for the treatment and prevention of bacterial infections for the past 70 years.
Β-Lactams contain a four-membered β-lactam ring with an amide group. This ring attacks penicillin-binding proteins (PBPs). These are the bacterial proteins responsible for bacterial cell wall synthesis via peptidoglycan linkages. By targeting penicillin-binding proteins, beta-lactams inhibit cell wall synthesis, leading to bacterial lysis.

What is the difference between LACTAM ANTIBIOTICS AND BETA LACTAMASE?
Beta-lactam antibiotics are antibacterial agents that contain a beta-lactam ring in their chemical structure. This is why they are called beta-lactam antibiotics. The beta-lactamases are the enzymes that are produced by bacteria and attack the four-membered beta-lactam ring, which is a core component of beta-lactam antibiotics. Hence, it leads to the inactivation of beta-lactam antibiotics.
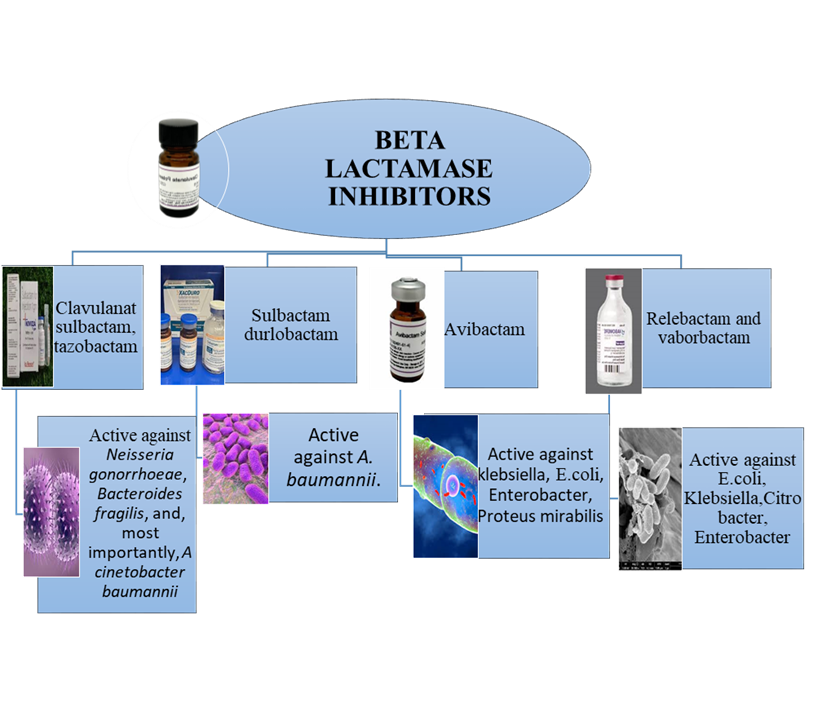
BETA LACTAMASE INHIBITOR:
Beta-lactamases are those antibacterial agents that inhibit the activity of beta-lactamase enzymes. These antibiotics can be given in combination with beta-lactam antibiotics to prevent antibiotic resistance.
Example:
v Clavulanic acid,
v Sulbactam, and
v Tazobactam,
v Avibactam (newer)
v Vaborbactam (newer)
CLASSES OF BETA LACTAM ANTIBIOTICS:
The following are the major classes of beta-lactams
- Penicillins (e.g., penicillin G, amoxicillin, flucloxacillin)
- Cephalosporins (1st–5th generations; e.g., cefazolin, ceftriaxone, ceftazidime, cefepime)
- Carbapenems (e.g., meropenem, imipenem)
- Monobactams (aztreonam)
INDICATIONS:
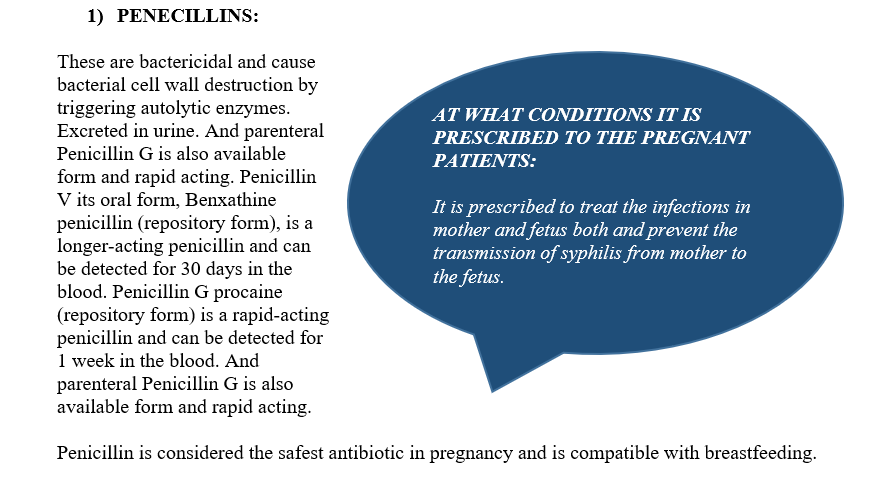
- Natural Penicillin is used to treat penicillin-susceptible Streptococcus infections, meningitis, streptococcal pharyngitis, endocarditis, N. meningitidis, and syphilis.
- Beta-lactamase–Resistant Penicillins like Oxacillin, Nafcillin, and Dicloxacillin are the First-line agents for methicillin-susceptible Staphylococcus aureus MSSA, covering skin, soft-tissue, and other serious MSSA infections.
- Aminopenicillins are used for upper respiratory infections caused by Enterococcus faecalis and Listeria.
- Aminopenicillin + Beta-Lactamase Inhibitor Combinations are used for the treatment of upper respiratory tract infections, mixed aerobic–anaerobic, and intra-abdominal infections.
- Ureidopenicillins (Piperacillin-Based) are active against resistant gram-negative organisms, including Pseudomonas aeruginosa. Mostly used to treat hospital-acquired infections.
ADVERSE EFFECTS:
Penicillins can cause:
· Hypersensitivity reactions in susceptible individuals, including rashes and, rarely, severe reactions such as anaphylaxis.
· Gastric effects like black hairy tongue, and less frequently cause diarrhea.
· High doses can cause neurotoxicity, pain at the site of injection, and nephritis.
2) CEPHALOSPORINS:
Cephalosporins are the β-lactam antibiotics that destroy bacteria by inhibiting the activity of enzymes involved in bacterial cell wall synthesis.
GENERATIONS AND THEIR INDICATIONS:
According to their spectrum of activity, they are categorized into different generations
1. First-generation cephalosporins treat skin infections and soft tissue infections that are caused by methicillin-susceptible Staphylococcus aureus MSSA. And also used for surgical prophylaxis to prevent infections.
2. Second-generation agents are used for the management of upper respiratory infections and also used for gynecologic infections and perioperative prophylaxis.
3. Third-generation cephalosporins are used for the treatment of community-acquired pneumonia, meningitis, UTIs, gonorrhea, endocarditis, and severe Lyme disease.
4. Anti-pseudomonal cephalosporins are the highly active agents against nosocomial pneumonia, meningitis, and complicated intra-abdominal or urinary tract infections.
5. Anti-MRSA cephalosporins treat community- and hospital-acquired pneumonia and skin and soft tissue infections.
Cephalosporins are considered safe during pregnancy and are contraindicated in breastfeeding mothers because they may cause alterations in the microflora of infants.
ADVERSE EFFECTS:
The adverse effects include:
· Mild hypersensitivity reactions
· Causes C. difficile diarrhea
· Lowering blood counts
· Irritation at the site of injection.
· Cefotetan can stimulate alcohol-related nausea and may increase bleeding risk.
3) CARBAPENEMS:
Carbapenems are bactericidal broad-spectrum beta-lactam antibiotics that contain a beta-lactam ring helps in opposing beta-lactamase enzymes.
Mechanism of resistance:
Pseudomonas aeruginosa and Acinetobacter baumannii, which produce carbapenemase enzymes that break down these drugs.
4) MONOBACTAMS:
These are the parenteral bactericidal beta-lactam antibiotics and having the aztreonam as the only drug in this class.
Aztreonam shows activity against aerobic gram-negative bacteria
It can be given in combination with aminoglycosides
INDICATION:
Used for treating meningitis patients allergic to beta-lactam, as in its chemical structure, it contains a beta-lactam ring isolated.
It can also be used for the treatment of other beta-lactam antibiotic-resistant infections
CONCLUSION
Beta-lactam antibiotics are considered the backbone of modern antimicrobial therapy due to their proven efficacious activity, wide safety margin with absolute potency, and broad clinical applications.
Their activity against PBPs and inhibiting bacterial cell wall synthesis makes them highly effective against a wide spectrum of pathogens. However, the increasing production of beta-lactamases by bacteria has led to rising resistance, making beta-lactamase inhibitors and newer drug combinations essential in current medical practice. Understanding the differences among penicillins, cephalosporins, carbapenems, and monobactams helps clinicians choose the most appropriate agent for each infection.
Although the antibiotic resistance is increasing rapidly but beta-lactam antibiotics still play their role against multiple bacterial infections and are irreplaceable in both community and hospital settings.
More importantly, always try to complete the antibiotic therapy even if your symptoms have been cured. Remembering that antibiotics are the effective agents against bacteria only can lead to the prevention of ANTIBIOTIC Resistance development.
Frequently Asked Questions (FAQs)
1. What are beta-lactam antibiotics?
Beta-lactam antibiotics are bactericidal drugs that contain a β-lactam ring and inhibit cell wall synthesis and causing lysis.
2. How do beta-lactams work?
Beta-lactam antibiotics work in 3 steps:
1) bind to penicillin-binding proteins (PBPs)
2) block peptidoglycan cross-linking,
3) Hence, weaken the bacterial cell wall, and cell lysis occurs.
3. How are beta-lactam antibiotics different from beta-lactamase enzymes?
Beta-lactam antibiotics are the drugs that are used to treat bacterial infections, whereas beta-lactamase enzymes are produced by bacteria that work against the β-lactam ring-containing agents and cause resistance.
4. What are the major classes of beta-lactam antibiotics?
Penicillins, cephalosporins, carbapenems, and monobactams.
5. Can beta-lactam antibiotics cause allergic reactions?
Yes. Reactions can be mild rashes to severe anaphylaxis, especially with Penicillins.
REFERENCES
v Bush K, Bradford PA. Epidemiology of β-Lactamase-Producing Pathogens. Clin Microbiol Rev. 2020 Feb 26; 33(2):e00047-19. Doe: 10.1128/CMR.00047-19. PMID: 32102899; PMCID: PMC7048014.