An abnormal state of heightened immune response which damages the normal tissues of the host body which causes an undesirable and adverse immune response to an antigen and further causes immune diseases including allergies and autoimmunity. There are many factors which influencing hypersensitivity.
Factors influencing hypersensitivity:
Genetic predisposition Environmental factors
Immune system dysfunction Previous exposure
Age Lifestyle factors
Medications Underlying health conditions
Occupational exposure Hygiene hypothesis
Types of Hypersensitivity:

Type I Hypersensitivity
- An immediate hypersensitivity reaction occurs when an antigen(allergen) binds to IgE on the surface of mast cells, resulting in the release of several mediators (e.g., histamine). The process begins with the sensitization to the antigen, which first induce the formation of IgE antibody.
- Type I Reaction occurs in two phases:
1. Sensitization phase
2. Activation phase
Phase 1: Sensitization phase

Phase 2: Activation phase
Upon exposure with the same allergen (antigen) cross-link IgE on mast cells, generating an intracellular signal that prompts mast cells to degranulate.

Degranulation
The release of wide variety of mediators of inflammation. There are 2 types of mediators.
1. Primary mediators
- Histamine
- Heparin
- Serotonin
- Cytokines and chemokines
2. Secondary mediators:
- Prostaglandins
- Leukotrienes
- Platelet-Activating factor
Clinical Manifestation:
Type I reaction result in vasodilation, increased capillary permeability, edema, vasoconstriction, bronchoconstriction, increased mucus secretion.
Symptoms are determined by location of allergens:
- Inhaled Allergens: Deposit in nasopharyngeal and bronchial tissue resulting in Allergic Rhinitis and Allergic Asthma.
- Ingested Allergens: Food allergy (symptoms include vomit, abdominal pain, dysphagia).
- Skin Allergens: Eczema, Itching, Swelling.
- Systemic: Anaphylaxis (shock, hypotension, wheezing, asphyxia, cardiac arrest).

Type II Hypersensitivity Reaction
- Hypersensitivity reaction mediated by IgM and IgG antibodies (Ab) that bind to:
- Intrinsic antigens on cell surfaces (RBCs)
- Extrinsic antigens (e.g., blood products, drugs)
- Ab-Ag binding results in cytotoxicity or abnormal cell function without cytotoxicity.
Mechanism:
These autoantibodies can cause various disease via two pathways.
- Cytotoxic pathway (cellular destruction & inflammation)
- Non cytotoxic pathway (physiological responses damage)
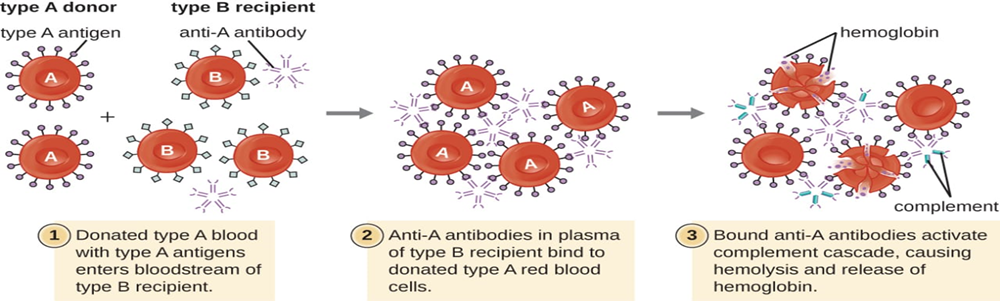
1. Cytotoxic pathway:
- Cellular destruction by neutrophils or macrophages.
- Fc region of the antibody activates the complement system (more than 30 proteins involve) through classical pathway.
It creates following responses:
- Inflammatory response:
- Chemotaxis factors (C3a, C4a, and C5a) produced.
- Invite neutrophils, damage tissues
- Membrane attack complex (MAC):
- (C5b and C6, C7, C8, C9) Attaches to cell membrane and make a ring or a circle which puncture in cell cause cell lysis.
- Example: ABO blood group incompatibility.
Antibody-dependent cellular cytotoxicity (ADCC)
- Antibodies bind on antigen (Fab site).
- If antigen-Ab complex is too large to be phagocytosed, Fc receptors bearing effector cells, mainly natural killer cells are recruited.
- NK bind to Fc receptors of Ab, release toxic granules and cell lysis.
- Example: Tumors

2- Non cytotoxic pathway
- Antibody-mediated cellular dysfunction.
- Non-cytotoxic.
- Autoantibodies bind to cell-surface receptors to produce an abnormal activation/blockade of the signaling process.
- Regulate cell function without cell injury/inflammation.
- Examples: Myasthenia gravis (Ab causes blockade of acetylcholine receptor).
TYPE III: IMMUNE-COMPLEX HYPERSENSITIVITY
Deposition of immune complexes activate the complement system, polymorphonuclear cells are attracted to the site; inflammation and tissue injury occur.

Mechanism of Type III Hypersensitivity
- Ag+ Ab form immune complexes of different sizes.
- Large complexes can be cleared by macrophages.
- Insertion of immune complexes into small blood vessels, joints and glomeruli.
- Immune complexes deposition activates the complement system and macrophages and neutrophils are attracted to the site, leading to inflammation and tissue injury.
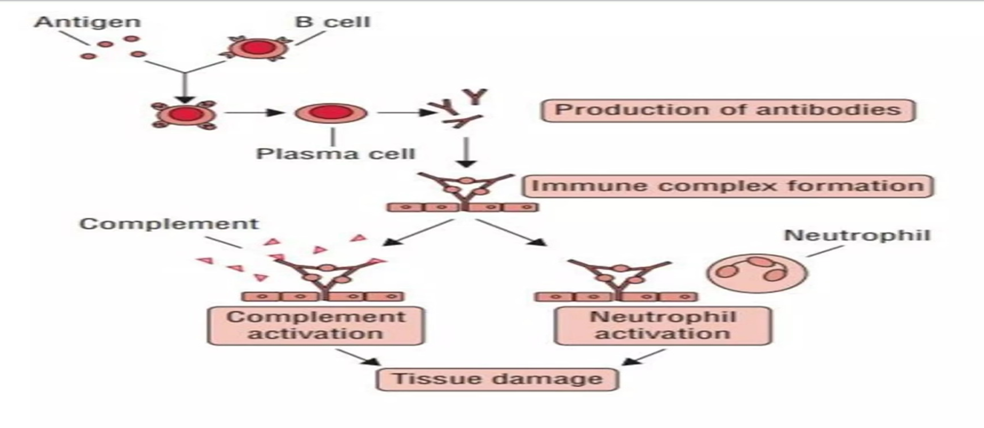
- Immune complexes activate C3a and C5a components.
- Degranulation of mast cells release histamine.
- C3a and C5a act as chemotactic factors for neutrophils.
- C3b act as opsonin by binding with the immune complex.
- Neutrophil binds to the C3b coated immune complex, and attempts to phagocytose but it is not possible,
- So, lytic enzymes are released to destroy immune complex.
- Resulting in hypersensitivity reaction.

Forms of Type III Hypersensitivity
- Two typical type III hypersensitivity reactions:
1) Localized Type III hypersensitivity reaction:
Arthus reaction
2) Generalized Type III hypersensitivity reaction
serum sickness.
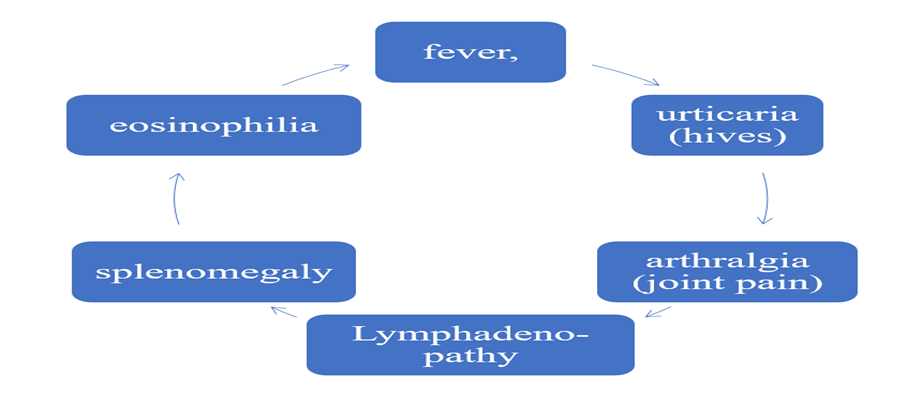
SERUM SICKNESS
- Systemic inflammatory response triggered by the deposited immune complexes.
- Injection of foreign serum or certain drugs.
- Slow excretion of the antigen; antibody production.
- Ag-Ab presence leads to immune complexes formation.
In modern times; drugs, such as penicillin is common cause
Type IV Hypersensitivity Reaction
- Type IV hypersensitivity is mediated by T cells and macrophages
- Reaction occurs at least 1–3 days after the initial exposure
Activation → Recruitment → Response
- Delayed-type hypersensitivity (DTH)
Mechanism
- Activation of CD4 + T cells by tissue APCs can lead to tissue damage via two mechanisms:
- 1. Cytokine-mediated inflammation.
- 2. Direct cell killing by CD8 + cytotoxic T cells (CTLs).
CYTOKINE-MEDIATED INFLAMMATION

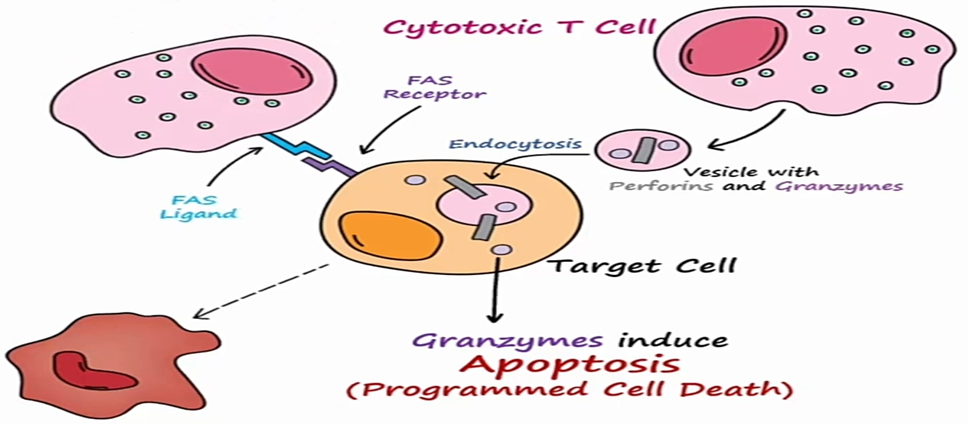
CYTOTOXIC T CELL MEDIATED TYPE IV HYPERSENSITIVITY
- Target cell is recognition
- Release of vesicle that is endocytosed by the target cell
- Perforins allow release of granzymes inside the cell
- Apoptosis
Cytotoxic cell may also bind to the FAS receptor utilizing a FAS ligand to activate apoptotic cell death.
Examples
- Type 1 Diabetes
- Rheumatoid Arthritis
- Graft Rejection
CONCLUSION
Overall, Hypersensitivity is an abnormal state of heightened immune response which is influences by many factors and it mainly damages the normal tissues of the host body and causes an undesirable and adverse immune response to an antigen and further causes immune diseases including allergies and autoimmunity Additionally, there are mainly four types of hypersensitivity and all of the types have different mechanisms. However, Type I, II and III are mediated by antibodies while Type IV is cell mediated immune response.
FAQs
- WHAT ARE THE COMMON SYMPTOMS OF HYPERSENSITIVITY?
The common symptoms include coughing, sneezing, runny nose, irritated eyes and rashes.
- CAN HYPERSENSITIVITY BE FATAL?
Yes, in rare cases hypersensitivity can lead to anaphylaxis which can be life threatening.
- CAN HYPERSENSITIVITY BE INHERITED?
Yes, it can be inherited.
- AT WHAT AGE MOSTLY HYPERSENSITIVITY DEVELOP?
Most allergies develop in childhood but they can be reactivated later in any age of the life.
- WHAT IS THE MOST COMMON EXAMPLE OF HYPERSENSITIVITY REACTION?
Allergic rhinitis is the most prevalent allergic disease.






