
PHOSPHINE GAS:
- Phosphine gas is a highly toxicant gas. It is colorless gas. Its chemical formula is PH3 and molecular weight is 34.
- It is odorless gas in its pure form, however commercial grade phosphine often has a strong unpleasant smell similar to rotting fish.
- It is highly flammable can easily catch fire or explode in air. To prevent this it’s usually combine with carbon dioxide to minimize its flammability.
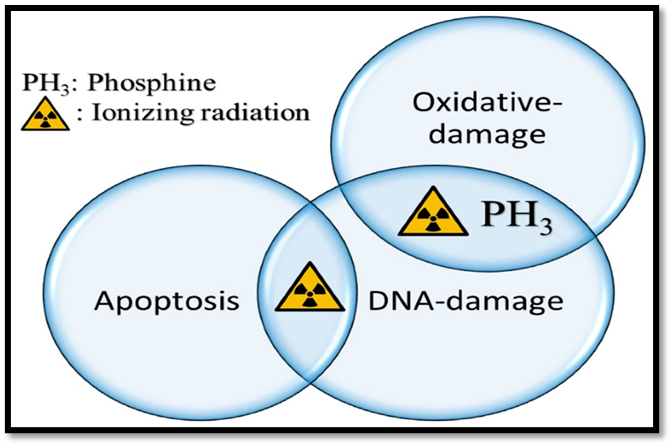
TOXICITY MECHANISM:
Phosphine kills insect by damaging their cell’s energy production system, specifically the mitochondrial electron transport chain. When phosphine is oxidized, it produces highly reactive molecules that damage insects, leading for their death. This mechanism is different from other insecticides.
APPLICATION OF PHOSPHINE GAS:
- Phosphine gas is used as fumigant to protect the stored grain against insects.
- Phosphine gas is highly toxic to oxygen-dependent organisms but not to anaerobic or dormant organisms. This property makes it an effective pest control agent for grain storage without compromising grain quality.
- Phosphine breakdown into harmless substances that are easily absorb by cells. It’s ease of use, effectiveness and low cost made it a widely used pesticide for grain traded globally for human consumption.
LETHAL DOSE IN HUMAN:
In human beings the lethal dose is greater than 7ppm.
LETHAL DOSE IN ANIMALS:
In mice the lethal dose is 9mg/m3.
TOXICITY OF PHOSPHINE GAS:
- Exposure routes:
- Oral (intentionally by ingestion of aluminum phosphide palettes)
- Inhalation (accidentally by inhalation).
CLINICAL SYMPTOMS OF PHOSPHINE TOXICITY:
Common Symptoms of Phosphine Inhalation
The signs and Symptoms of phosphine poisoning can appear suddenly and vary depending on the dose, how you were exposed (oral , inhalation or dermal) and how much time has passed. After inhalation exposure, patients commonly have:
- Airway irritation
- Breathlessness
- Dizziness
- Fatigue
- Chest tightness
- Headache
- Nausea
- Vomiting
- Diarrhea
- Ataxia (loss of coordination)
- Numbness
- Tingling (paresthesia)
- Tremor
- Muscle weakness
- Double vision (diplopia)
- Jaundice
Severe Inhalation Toxicity Symptoms
- Acute respiratory distress syndrome (ARDS)
- Cardiac failure
- Cardiac arrhythmias
- Convulsions
- Coma
- Hepatotoxicity (liver damage)
- Nephrotoxicity (kidney damage)
Mild Ingestional Poisoning Symptoms
- Human toxicity can occur through ingestion of aluminium phosphide or inhalation of phosphine gas release from fumigated grains.
- In human case studies of suicidal attempts by ingestion of aluminium phosphide palette has been reported. The ingestion of aluminium phosphide palettes that lead to the release of phosphine gas in the stomach, which is then rapidly absorbed through the gastrointestinal tract.
- Nausea
- Vomiting
- Diarrhea
- Headache
- Abdominal discomfort or pain
- Rapid heart rate (tachycardia)
Moderate to Severe Ingestional Poisoning Symptoms
- Gastrointestinal issues
- Cardiovascular problems
- Respiratory distress
- Neurological symptoms
- Hepatic (liver) failure
- Renal (kidney) failure
- Disseminated intravascular coagulation (blood clotting disorder)
Neural/Behavioural effects : Phosphine exposure causes initial agitation and convulsions in humans and hyperactivity and twitching in animals. Later, lethargy in humans and necrosis or anesthesia in animals. This is due to phosphine’s effect on acetylcholine, a neurotransmitter:
- Phosphine suppresses acetylcholine esterase, leading to overactive acetylcholine signalling. This causes hyperactivity and potentially excitotoxicity. A study on rats provided the strongest evidence that excessive acetylcholine signaling, caused by inhibition of the esterase, contributes to phosphine toxicity. Rats exposed to lethal dose of Phosphine,
- Administering pralidoxime (which blo acetylcholinesterase inhibitors) and atropine (which blocks muscarinic receptors) significantly reduced phosphine toxicity.
- Nine rats treated with both drugs lived 2.5 times longer than control rats, and six rats survived phosphine exposure entirely.
HISTOPATHOLOGICAL FIDNINGS OF ACUTE PHOSPHINE POISONING

ANTIDOTE:
There is no specific antidote for phosphine toxicity. Treatment is primarily focused on supportive care, managing symptoms, and providing respiratory and cardiovascular support.
MANAGEMENT:
If someone is exposed to phosphine gas, then
1. Move them to fresh air immediately.
2. Wash their skin and eyes with plain water as soon as possible to prevent further absorption.
If aluminium phosphide palettes ingested then
- Ingestion was confirmed by history and typical odor of aluminium phosphide. Number of tablets ingested or amount of powder used, date of opening of container, nature of poisoning (suicidal or accidental), complaints, clinical characteristics and laboratory data were recorded at the time of admission.
- GI decontamination is effective within 1-2 hours of ingestion.
- Gastric lavage was performed with diluted potassium permanganate (1:10000 dilution), coconut oil, sodium-bicarbonate and activated charcoal.
- Activated charcoal (100g) may be used within 1 hour of ingestion.
- Airway protection was given before gastric lavage in required patients.
- Supportive treatment included intravenous (IV) fluids, vasopressors and inotropic drugs, sodium-bicarbonate infusion, magnesium sulfate infusion and proton pump inhibitors. Close monitoring of hemodynamic parameters, urine output, arterial blood pressure and arterial blood gas should be regularly done.
STUDENT 02 – CASE studies
CASE 01 – Emergency department (ED) of Notre Dame des Secours University Hospital Center-Lebanon
A 37 years old male brought to emergency department because he had consumed 5 pesticide tablets before one hour to commit suicide. He was conscious but anxious.
Vitals indicated
- A slow heart rate (65 bpm)
- Low blood pressure (90/50 mmHg)
- Rapid breathing (28 breaths per minute)
- Low oxygen levels (92% on room air)
- A normal body temperature (36.8°C)
He was agitated, had a reduced level of consciousness (GCS score of 10), and his pupils were reactive. His skin was warm and dry. An ECG showed an irregular heartbeat with abnormal heart patterns (atrial fibrillation, ST depressions, and T wave inversions).
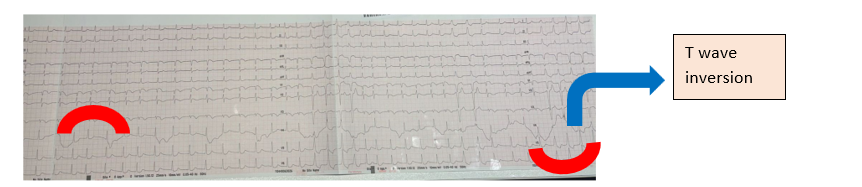
| T wave inversion |
Immediately intravenous fluids and oxygen was given to the patient. Activated charcoal was administered with 1g/kg. The patient’s condition deteriorated shortly after. He experienced a hazardous drop in oxygen levels (57%), a further fall in blood pressure (70/50 mmHg), and a deterioration in awareness (GCS score of 4). His body was getting dangerously acidic, according to blood tests that revealed severe metabolic acidosis.
In order to assist him breathe, doctors put him on a ventilator. They also changed his oxygen levels and gave him sodium bicarbonate to balance his acidity. The acidity of his blood persisted in spite of these measures. Despite receiving more fluids and sodium bicarbonate, his blood pressure remained low, necessitating the use of vasopressor drugs. Severe poisoning was confirmed by his blood tests, which also revealed renal damage and a significant anion gap acidosis.[1]
Case 02 – Progressive and worsening condition of “Phosphine poisoning”
Department of Poisoning and Occupational Diseases, Emergency Medicine, Qilu Hospital of Shandong University, Jinan 250012, China
Phase I – On 22 July 2022 a case has arrived in ED with a chief complain of nausea and chest tightness. The basic or routine examination has done including (bloodwork, liver/kidney function, ECG) these were normal enough that no treatment was given.The patient history revealed that he has performed fumigation in his garden.
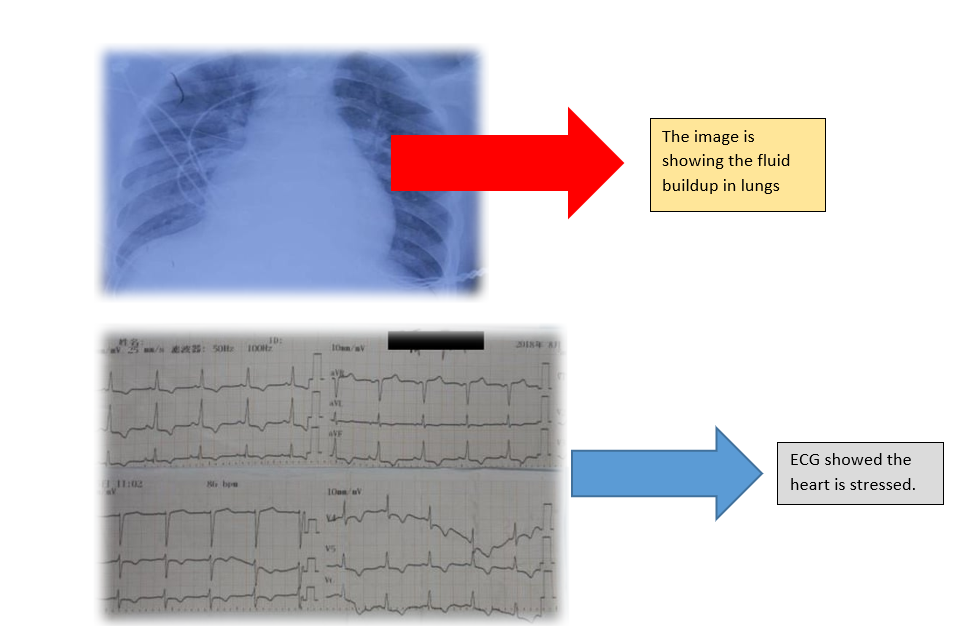
Phase II– On next day he again fumigated his garden. While performing fumigation again, the patient collapsed, lost consciousness, and exhibited foaming at the mouth—classic signs of severe poisoning.He was comatose as well when arrived hospital sufficient supportive treatment has been provided including :
Endotracheal intubation for airway protection. Mechanical ventilation due to respiratory failure. IV fluids to stabilize circulation and prevent shock.
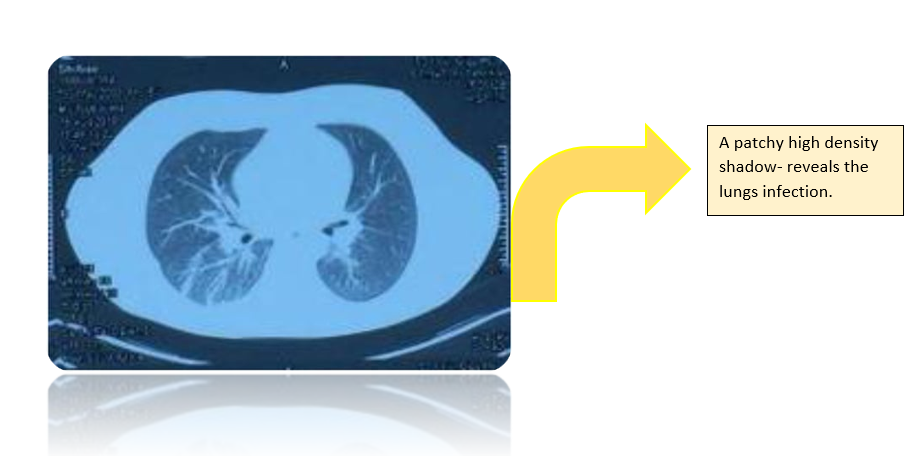
X ray has revealed inflammatory victims in lungs and showed fluid buildup in lungs, enlarged heart walls might be due to stress on heart.
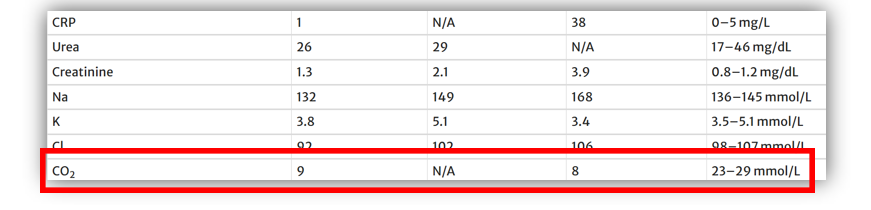
Phase III– The patient’s condition was worsening hence he was transferred to ICU for advance treatment. LFTs, PT and other laboratory testing were out of range showed patient’s organs declined in their functionalities.
Treatment included:
- Hemoperfusion (blood filtration): To remove toxins from the bloodstream.
- Norepinephrine and epinephrine: To maintain blood pressure and stabilize cardiovascular function.
- Steroids (methylprednisolone): To reduce severe inflammation.
- Sedation (midazolam): To keep the patient in calm.
Then on 29 July – 14 August patient was showing gradual improvement with stabilize lab reports including LFTs, PT etc.
On the next day patient suffered from a high fever with coughing and yellow phlegm directing the lung infection. Sputum samples were collected and it was revealed the presence of Pseudomonas aeuroginosa and E.coli in it. Hence an antibiotic Imipenem was prescribed for treatment.The patient was discharged after his fever resolved and breathing stabilized.[2]
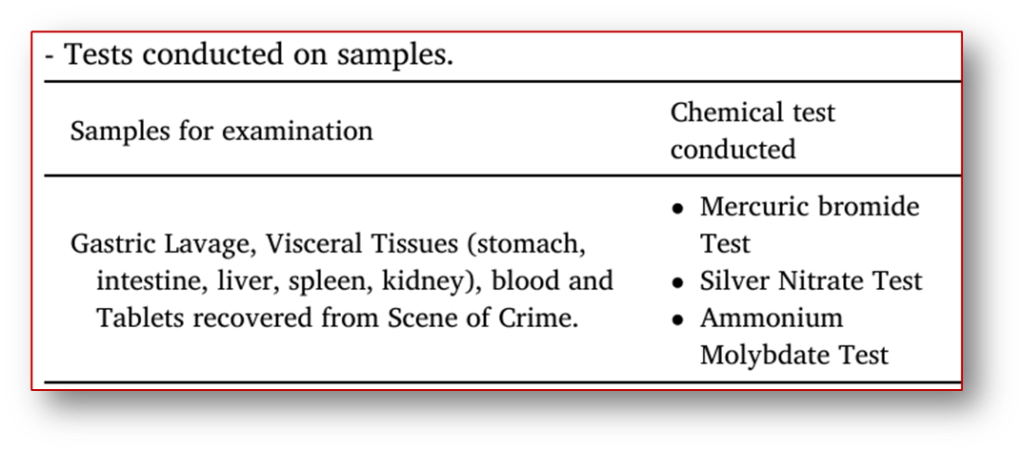
Case 03 A mysterious case with forensic diagnosis
Forensic Science Laboratory, Rohini, Delhi, India
In the month of July several cartons were stored in warehouse two persons aged above 20 years were slept for a night and on next morning they found unconscious.
It was initially suspected as case of food poisoning but total out of four only two showed symptoms. These were slept in the middle of the warehouse while the two were slept on the upstairs. Warehouse lacked proper ventilation and a peculiar smell was noticed.
Upon investigating the area of warehouse some gray tablets were found with a garlic like odor, after analyses of tablets it was claimed as “Aluminum phosphate tablets”.
ALP reacts with moisture to produce highly toxic phosphine gas. They inhaled phosphine gas from leaked containers of ALP behind the cooler.
The cooler’s missing panels and running motor created suction, intensifying the spread of the gas. The moist and humid environment (common in July) further accelerated the release of phosphine gas.
The victims, sleeping near the cooler, inhaled the toxic gas, leading to symptoms like restlessness and vomiting, followed by respiratory failure.[3]
REAL CASE – PART 03
REAL CASE SCENARIO – A CRUCIAL DIAGNOSIS (AKUH,Karachi)
A case of “Phosphine poisoning” was reported at Aga Khan University Hospital, Karachi, Pakistan. Three young children were brought to the Emergency Department:
- 8 years old – A girl
- 5 years old – A boy
- 3 years old – A boy
All three children exhibited symptoms of diarrhea, vomiting, and drowsiness. Their parents revealed that 25 unlabeled insecticide tablets, with a garlic-like smell, had been used in their rooms.
The eldest child passed away on the way to the hospital. The 5-year-old boy was admitted to the ICU, while the 3-year-old boy was admitted to the Pediatric Ward. Based on the symptoms and history provided, the medical team initially treated the children for organophosphate poisoning.
The 3-year-old boy showed improvement and was discharged. However, he died at home within 10 hours. This unexpected death prompted the medical team to reconsider the diagnosis, as organophosphate poisoning typically does not cause delayed effects.
Further examination of the surviving 5-year-old boy revealed symptoms of cardiac dysfunction, including delayed capillary refill and reduced ejection fraction. He was subsequently transferred to the Cardiac Unit and treated with dopamine infusion.
The parents brought the suspected insecticide tablets for analysis. It was found that the tablets contained Aluminum Phosphide (ALP).
ALP reacts with stomach acid and water to release lethal phosphine gas, which causes severe cardiac and pulmonary abnormalities. Definitive treatment was initiated with methylprednisolone, dobutamine, oxygen, and nebulization. After 48 hours, the child’s heart function improved, and he was discharged following a period of observation.
Case : 02 Another case scenario of Agha Khan
An 8 kg child who was a year and four months old complained of abrupt onset vomiting that started in the morning.
Symptoms:
She had no fever, loose stools, or other accompanying symptoms. Upon inspection, she appeared lifeless, tachypnea, dehydrated, and breathing acidotically. Despite her weak pulses and delayed CRT.
Labs:
- Blood pressure of 90/53 mm Hg
- Saturation level of 99% at room air.
- ABGs showing pH 7.46, PCO2 24.20 mmHg, PO2 93.10 mmHg, bicarbonate 16.90 mEq/L, base excess -4.9 mEq/L
- O2 sat 97.60%.
- CBC, LFT, electrolytes and PT/INR were normal
- lactic acid was 2.2 mmol/L.
An x-ray of the chest revealed evidence of pulmonary edema.
The patient also experienced sinus arrhythmia while in the emergency department, and the ED echocardiography revealed a moderately dilated left ventricle without hypertrophy and an ejection fraction of 34%. After being admitted to the intensive care unit, the patient received high flow oxygen and magnesium sulfate every six hours under close observation.
Treatment – Epinephrine and milrinone, as well as diuretics and ACE inhibitors, were introduced as double inotropic support.
Multiple organ involvement from phosphorus toxicity results in pulmonary edema, liver failure, heart failure, and renal failure. When aluminum phosphide or phosphine poisoning occurs, cardiac arrhythmias (such as bradycardia, ventricular tachycardia, and cardiac failure) are the most frequent cause of death.
The family used aluminum phosphide tablets for fumigation purposes, but they were not properly counseled regarding the safe removal of the gases from the rooms or the duration of the fumigation because they purchased the tablets over-the-counter from a vendor and were totally ignorant of the potential side effects.[4]
REFRENCES:
1. Edde, P., et al., The first reported mortality from aluminum phosphide poisoning in Lebanon: a case report. International Journal of Emergency Medicine, 2024. 17(1): p. 18.
2. Shi, L., et al., Case Report: Acute Intoxication from Phosphine Inhalation. International Journal of Environmental Research and Public Health, 2023. 20(6): p. 5021.
3. Singh, R.K., et al., Mysterious death due to accidental inhalation of phosphine – A unique case study. Forensic Science International: Reports, 2022. 5: p. 100264.
4. Hena, Z., et al., Aluminum phosphide poisoning: Successful recovery of multiorgan failure in a pediatric patient. International Journal of Pediatrics and Adolescent Medicine, 2018. 5(4): p. 155-158.


