Anemia is the most common blood disorder; around 30% of the world’s population is anemic. It is defined as the condition in which the number of red blood cells or the concentration of hemoglobin is lower than normal and reported as low hemoglobin or hematocrit.
Hemoglobin, a protein in RBCs, is responsible for transporting oxygen from the lungs to the rest of the body. In anemia, deficiency in hemoglobin and reduced transport of sufficient oxygen to the tissues and organs ultimately lead to fatigue, weakness, dizziness, and shortness of breath.
Normal hemoglobin levels vary by age, gender, and physiological conditions.
Men: 13.8–17.2 g/dL
Women: 12.1–15.1 g/dL
Children: 11–16 g/dL
A hemoglobin level below these ranges is considered anemic.
Classification of Anemia:
Depending on the size of the red cells (MCV), anemia can be classified as:
- Microcytic Anemia: in which MCV (Mean corpuscular volume) is less than 80fL
- Normocytic Anemia: in which MCV (Mean corpuscular volume) is between 80-100fL.
- Macrocytic Anemia: in which MCV (Mean corpuscular volume) is greater than 100fL.
Types of Anemia based on etiology:
Anemia can be classified into the following types based on the underlying factors:
- Iron Deficiency Anemia:
It is the most prevalent type of anemia; occurs because of the low iron levels. Inadequate iron intake, iron loss, extensive blood loss, GI bleeding, malabsorption, and increased physiological demands can lead to iron deficiency Anemia.
- Clinical Features:
Fatigue, pallor, brittle nails, glossitis
- Key Diagnostic Features:
Low iron, low ferritin, elevated TIBC
2.Megaloblastic Anemia:
This occurs as a result of Vitamin B12 or Folic acid deficiency, or from disturbances in folic acid metabolism. This deficiency will lead to high plasma levels of homocysteine, and impaired DNA synthesis which results in impaired red blood cell production.
Significant vitamin B12 deficiency can lead to neurological disease in up to 40% of cases, with the chief pathological findings such as focal demyelination affecting the spinal cord, peripheral nerves, optic nerves, and cerebrum.
- Clinical Features:
Neuropathy, malaise breathlessness, weight loss, macrocytic RBCs, Glossitis (inflamed tongue)
- Key Diagnostic Features:
Low serum B12 levels, Elevated MCV
3. Hemolytic Anemia:
Hemolysis refers to the destruction of the RBCs. In hemolytic anemia, premature destruction of the RBCs occurs (Normal lifespan: 120 days). To compensate the bone marrow increases the proportion of red cells produced but anemia occurs when the rate of destruction exceeds this increased production rate. Hemolytic Anemia may occur due to underlying autoimmune diseases, genetic conditions, or infections.
- Clinical Features:
Jaundice, dark urine, splenomegaly
- Key Diagnostic Features:
Low Hemoglobin and hematocrit, elevated bilirubin
4.Aplastic Anemia:
In aplastic anemia, bone marrow failure leads to a decreased production of red blood cells. It is prevalent in people exposed to toxic chemicals, radiation, or viral infections.
- Clinical Features:
Frequent infections, unexplained bleeding, and bruising, increased heartbeat.
- Key Diagnostic Features:
Pancytopenia (low RBC, WBC, and platelet counts), Bone marrow biopsy
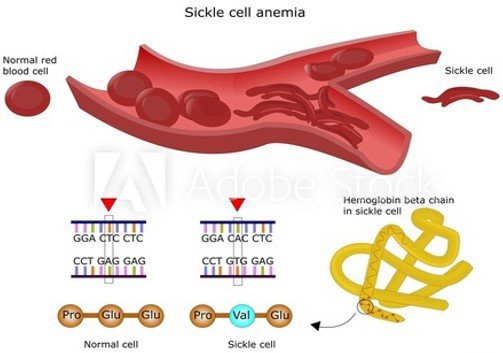
5. Sickle Cell Anemia:
It is a type of anemia in which the RBCs become Sickle-shaped. It genetic disorder that occurs because of the point mutation in which glutamic acid is replaced with valine at position 6 of the beta-globin polypeptide chain. In sickle cell anemia, there is a high risk of sudden cardiovascular death because of the blockage of the blood flow.
- Clinical Features:
Painful vaso-occlusive crisis, swelling in hands and feet, eye damage, leg ulcers, pulmonary and heart diseases
- Key Diagnostic Features:
- Hemoglobin electrophoresis: presence of HbS (sickle hemoglobin)
- Sickle cell test: positive for sickle cells
- Low hemoglobin and hematocrit level
6. Anemia of Chronic Disease:
This type of anemia occurs because of long-term medical conditions (chronic kidney disease, cancer, autoimmune diseases) or chronic inflammations (e.g., infection, malignancy, autoimmune diseases) affecting RBC production.
- Clinical Features:
Fatigue, shortness of breath, weakness
- Key Diagnostic Features:
Serum iron normal or decreased, serum ferritin normal or elevated, TIBC normal or decreased
7. Sideroblastic Anemia:
Sideroblastic anemia is a rare genetic disorder characterized by the accumulation of iron in the mitochondria of red blood cell precursors, leading to defective heme synthesis and anemia.
- Clinical Features:
- Pallor, Jaundice, Enlarged spleen, Recurrent infections, Iron overload
- Key Diagnostic Features:
- Dimorphic anemia (mix of normocytic and microcytic cells), Bone marrow biopsy (revealing ringed sideroblasts), Elevated serum iron, transferrin saturation, and ferritin levels
Symptoms of Anemia
The symptoms of anemia vary with the severity and underlying cause. Common symptoms include:
- Fainting and Fatigue
- Shortness of breath and weakness
- Pale or yellowish skin and eyes
- Muscular weakness
- Dizziness or lightheadedness
- Cold hands and feet
- Chest pain, angina, or irregular heartbeat
- Headaches and difficulty concentrating
- Brittle nails and hair loss
Diagnosis of Anemia:
Anemia can be diagnosed through various laboratory tests which include the following:
- Complete Blood Count (CBC): It measures hemoglobin levels, RBC count, and hematocrit levels.
- Peripheral Blood Smear: Through blood smear analysis, the shape and size of red blood cells are examined (normocytic, microcytic, or macrocytic).
- Iron Studies: It is performed to check:
- Serum ferritin: It is a measure of iron stores in tissues and is the best single test to confirm iron deficiency.
- Plasma iron and total iron binding capacity (TIBC): These are the measures of iron availability; hence they are affected by many factors besides iron stores.
- Transferrin: It is the binding protein for iron.
- Vitamin B12 and Folate Tests: These tests are performed to determine underlying vitamin deficiencies.
- Bone Marrow Biopsy: It is performed in suspected cases of bone marrow disorders.
- Genetic Testing: Genetic testing is performed for genetic disorders like sickle cell anemia or thalassemia.
Treatment of Anemia
The treatment plan for anemia entirely depends on its etiology and the severity of the complications:
- Iron Supplements:
- Oral Ferrous sulfate tablets are to be continued for 3–6 months to replete iron stores.
- Intravenous iron therapy (with iron isomaltose and iron carboxymaltose) is preferred in severe anemia cases (Hb<9MG/dL) or when oral iron therapy is not tolerated.
- Dietary Changes: Include iron-rich foods in the daily diet plan like spinach, red meat, beans, and fortified cereals.
- Vitamin C Intake:
Increase Vitamin C (citrus fruits, bell peppers, tomatoes) intake because it enhances iron absorption.
3. Vitamin B12 Injections or Supplements:
Vitamin B12 and folic acid deficiency can be managed with Folic Acid Supplements and increased dietary intake (leafy greens, eggs, dairy, fortified grains).
4. Blood Transfusions:
Blood transfusion may be required in severe cases of anemia to maintain the RBC levels.
5. Bone Marrow Transplant: It is a potential cure in cases of aplastic and sickle cell anemia.
6. Immunosuppressive Therapy: It may be required to prevent immune attacks on bone marrow.
7. Pain management: To reduce the painful bouts of sickle cell anemia; NSAIDs and opioids may be required.
8. Erythropoietin Injections: To stimulate RBC production in kidney disease patients.
9. Treatment of Underlying Condition: In anemia of chronic disease, the treatment plan should cover the management of the underlying disease.
Prevention of Anemia:
Preventing anemia involves maintaining a healthy diet and lifestyle by:
- Iron-rich foods: Red meat, poultry, seafood, leafy greens, nuts, and seeds.
- Vitamin B12 & Folate: Dairy, eggs, fortified cereals, legumes.
- Avoid Excessive Tea/Coffee: They inhibit iron absorption.
- Regular Health Checkups: Monitor hemoglobin levels, especially for those at risk.
- Managing Chronic Diseases: Proper treatment of conditions like kidney disease can prevent anemia.
Conclusion:
Anemia is a complex and multifaceted disorder with various etiologies, ranging from nutritional deficiencies to chronic diseases and inherited disorders. It is characterized by reduced RBCs and Hemoglobin levels. Prompt diagnosis and appropriate management are crucial for improving quality of life and preventing complications. It is essential to maintain a balanced diet, seek medical care timely, and manage the underlying conditions; this can help prevent and treat anemia effectively.
FAQS:
- What is anemia?
Anemia is the most common blood disorder where there is decreased red blood cell count or hemoglobin, leading to reduced oxygen supply to tissues.
2. What are the Chief Clinical features of anemia?
Fatigue, dizziness, pallor, shortness of breath, and irregular heartbeat.
3. Who is at risk of developing anemia?
Women (especially during pregnancy), children, people with chronic illnesses, and those with poor diets.
4. How is anemia diagnosed?
Anemia can be diagnosed through blood tests like a Complete Blood Count (CBC), iron studies, and vitamin level tests.
5. Can anemia be treated?
Yes, anemia can be treated. Treatment of anemia depends on the etiology and may include iron or vitamin supplements, dietary changes, medications, or blood transfusions (in severe cases).





