Heavy metal poisoning is a serious and often overlooked health issue that can devastate individuals and communities. Heavy metals like lead, mercury, arsenic, and cadmium are naturally occurring elements, but when they accumulate in the body in toxic amounts, they can cause significant harm. The risk of heavy metal poisoning is particularly high in countries like Pakistan, where industrial pollution, inadequate regulation, and a lack of public awareness contribute to widespread exposure.
What is Heavy Metal Poisoning?
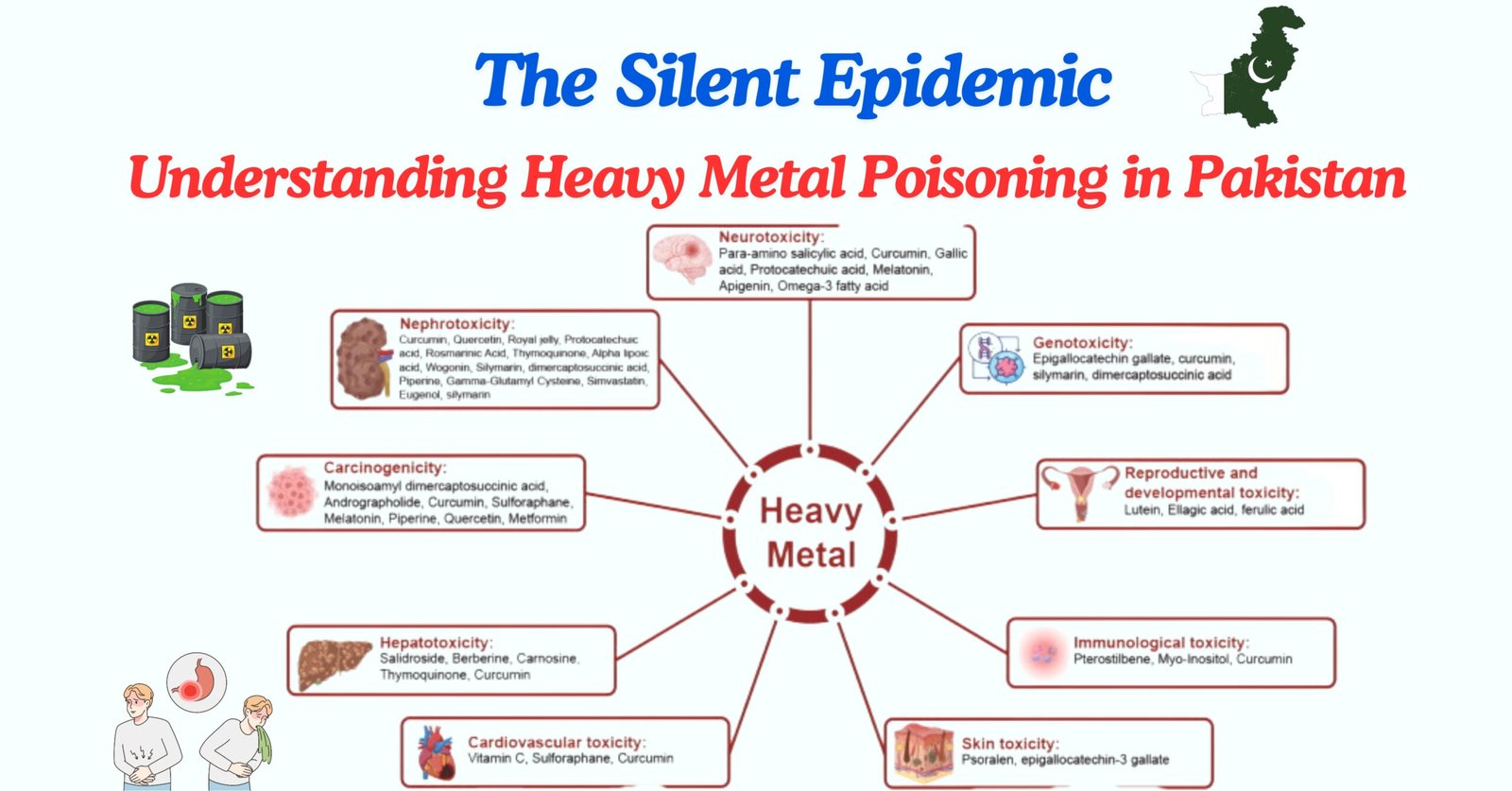
Heavy metal poisoning occurs when toxic levels of heavy metals accumulate in the body, either through ingestion, inhalation, or skin contact. These metals can disrupt vital biological processes by binding to proteins and enzymes, leading to a wide range of health problems. The symptoms of heavy metal poisoning can vary depending on the metal involved and the level of exposure, but they often include neurological, gastrointestinal, and cardiovascular issues.
For example, lead poisoning can cause cognitive impairments, developmental delays in children, and hypertension in adults. Mercury poisoning is known for its neurotoxic effects, leading to tremors, memory problems, and even vision loss. Arsenic, often found in contaminated drinking water, is a potent carcinogen and can cause skin lesions, respiratory issues, and an increased risk of cancer. Cadmium, which can be absorbed through contaminated food or cigarettes, is associated with kidney damage and bone demineralization.
The Human Impact:
Take the example of a small village in Punjab, where families have relied on groundwater for generations. In recent years, residents began noticing unusual health issues, skin rashes, persistent coughs, and, most disturbingly, an alarming number of cancer cases. Upon investigation, it was revealed that their water supply was heavily contaminated with arsenic. For the people in this village, the daily act of drinking water had become a silent killer.
Or consider the informal e-waste recyclers in Karachi. Many of them are young men working in hazardous conditions, breaking down old electronics to extract metals like copper and gold. Without protective gear, they’re exposed to toxic fumes and dust that contain high levels of lead and mercury. Over time, these workers experience memory loss, tremors, and other neurological symptoms. But with limited job options, they continue this dangerous work, unaware of the long-term damage to their health.
These stories are not isolated incidents. Across Pakistan, countless people are unknowingly exposed to heavy metals, leading to severe health consequences that are often misdiagnosed or left untreated.

Heavy Metal Exposure in Pakistan:
In Pakistan, heavy metal exposure is a growing concern due to rapid industrialization, unregulated mining, and the widespread use of pesticides and fertilizers. Industrial emissions, particularly from factories and tanneries, release significant amounts of heavy metals into the air, soil, and water. These pollutants can then enter the food chain, contaminating crops and livestock. Additionally, poor waste management practices and the use of leaded gasoline have contributed to elevated levels of heavy metals in the environment.
Arsenic contamination of drinking water is one of the most pressing issues in Pakistan. A significant portion of the population relies on groundwater for drinking and irrigation, and studies have shown that many wells in Pakistan exceed the World Health Organization’s (WHO) recommended limits for arsenic. Prolonged exposure to arsenic-contaminated water has been linked to a higher incidence of skin lesions, cardiovascular diseases, and cancers in affected communities.
In cities like Karachi, informal e-waste recycling is another critical source of exposure. Workers dismantle old electronics to extract valuable metals, often using methods that release toxic fumes and dust. These workers, who typically lack protective equipment, face severe health risks due to prolonged exposure.
Recommendations and Actionable Steps
Addressing heavy metal poisoning in Pakistan requires a comprehensive approach that includes stricter environmental regulations, public awareness campaigns, and improved healthcare services. First and foremost, it is crucial to enforce existing environmental laws and introduce stricter regulations on industries that emit heavy metals. Regular monitoring of air, water, and soil quality is essential to identify and mitigate sources of contamination.
Public awareness is another critical component of prevention. Educating communities about the risks of heavy metal exposure and how to reduce it—such as avoiding contaminated water sources, reducing the use of pesticides, and practicing safe recycling of e-waste—can help minimize exposure. Schools, healthcare providers, and local governments can play a vital role in disseminating this information.
Healthcare providers need better training to recognize the signs of heavy metal poisoning and to provide appropriate care. Chelation therapy, which involves administering agents that bind to heavy metals and help the body eliminate them, can be effective in treating heavy metal poisoning, but it is not widely available in Pakistan. Expanding access to such treatments, along with regular screening programs in high-risk areas, could significantly improve outcomes for those affected.
Conclusion
In conclusion, the pervasive issue of heavy metal poisoning in Pakistan represents a critical public health challenge that demands immediate and sustained action. The detrimental effects of heavy metals such as lead, mercury, arsenic, and cadmium on human health cannot be overstated, with communities across the nation facing dire consequences due to prolonged exposure. The stories from Punjab and Karachi are poignant reminders of the silent yet profound impact these toxins have on everyday lives, leading to severe health issues that are often overlooked or misdiagnosed. To combat this silent epidemic, a multifaceted approach is essential. Strengthening environmental regulations, enhancing public awareness, and improving healthcare responses are pivotal steps towards safeguarding the health of Pakistan’s population. Enforcing stringent controls on industrial emissions, promoting safer waste management practices, and ensuring regular monitoring of environmental contaminants are crucial. Additionally, public education campaigns can significantly contribute to reducing exposure risks by informing individuals about the dangers of heavy metals and practical prevention strategies. Moreover, enhancing the healthcare infrastructure to better diagnose, treat, and manage heavy metal poisoning is imperative. Expanding access to treatments like chelation therapy and increasing the availability of screening programs in high-risk areas can lead to better health outcomes and a more informed public. Addressing the issue of heavy metal poisoning with urgency and dedication is not just a matter of environmental or health policy but a fundamental aspect of social justice and human rights. Ensuring a healthier future for all citizens in Pakistan means taking decisive action now to mitigate this profound threat.
References:
- Agency for Toxic Substances and Disease Registry (ATSDR). (2019). Toxicological profile for lead. Retrieved from https://www.atsdr.cdc.gov/toxprofiles/tp13.pdf
- World Health Organization. (2018). Exposure to arsenic: A major public health concern. Retrieved from https://www.who.int/news-room/fact-sheets/detail/arsenic
- Khan, S., & Farooq, R. (2021). Heavy metal contamination in drinking water of Pakistan: A review. Environmental Science and Pollution Research, 28(10), 12445-12458. https://doi.org/10.1007/s11356-021-12367-9
- Fatmi, Z., & Rahman, A. (2020). E-waste management and its impact on health in Pakistan. Journal of Occupational and Environmental Medicine, 62(7), e342-e348. https://doi.org/10.1097/JOM.0000000000001908
- Arain, M. A., & Ashraf, M. (2019). Arsenic contamination of groundwater in Pakistan: A review of sources, health risks, and potential solutions. Environmental Science and Pollution Research, 26(9), 8491-8506. https://doi.org/10.1007/s11356-018-1325-6