Introduction:
Imagine feeling thirsty all the time, yet no amount of water quenches it. Or feeling tired even after a full night’s sleep. Millions of people worldwide aren’t just experiencing symptoms, but are actually facing daily struggles caused by diabetes. According to the World Health Organization (WHO), over 400 million people are currently living with diabetes, and the number continues to rise at an alarming pace. Diabetes is far more than just ‘high blood sugar’; it is a complex condition that silently affects almost every organ of the body, from the heart and kidneys to the eyes and nerves. The disease often develops silently, and many remain undiagnosed until complications appear.
What is Diabetes?
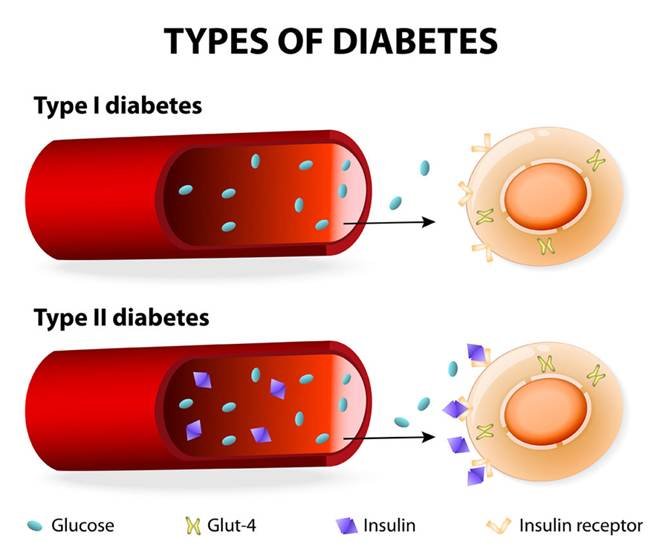
Diabetes mellitus (DM) is a chronic metabolic disorder characterized by persistent hyperglycaemia (high blood glucose levels) caused by insufficient insulin production, resistance to insulin, or a combination of both. There are three types of diabetes as under:
1. Type 1 Diabetes mellitus: It’s an autoimmune condition that results from the failure of the pancreas to produce enough Insulin. This occurs because the body’s immune system destroys insulin-producing cells in the pancreas. It usually develops in children or young adults and requires lifelong insulin therapy; therefore it was previously referred to as Insulin dependent Diabetes mellitus or Juvenile diabetes.
2. Type 2 Diabetes mellitus: This is the most common type of Diabetes mellitus, caused by insulin resistance and relative insulin deficiency. The primary causative factor is lifestyle such as obesity, poor diet, and lack of physical activity.
3. Gestational Diabetes: This is the third type of Diabetes mellitus which occurs during pregnancy due to hormonal changes and usually resolves after childbirth, though it increases the risk for mothers to develop Type 2 diabetes later in life.
Causes and Risk Factors of Diabetes
Diabetes mellitus does not develop overnight. A combination of genetic, environmental, and lifestyle factors increases the risk. In both of the common types of diabetes, environmental factors interact with genetic susceptibility to determine which people develop the clinical syndrome, and the timing of its onset.
ü Genetic Predisposition and Family History: The leading cause of Diabetes mellitus is genetic predisposition means having a parent or sibling with diabetes raises your chances.
ü Unhealthy Diet: High intake of sugary drinks, processed foods, and unhealthy fats contributes to insulin resistance.
ü Sedentary lifestyle: Obesity and physical inactivity are a major risk factor of Diabetes mellitus.
ü Age: Risk increases with age, especially after 45 years.
ü Pregnancy-related Risks: Women with gestational diabetes or polycystic ovary syndrome (PCOS) are at a higher risk of developing Type 2 Diabetes mellitus.
ü Other Factors: Hypertension, high cholesterol, and stress can also contribute to the pathophysiology of Diabetes mellitus.
Symptoms of Diabetes
Diabetes develops slowly, and can often be silent. Many people are unaware they have it until major complications occur. The common symptoms of untreated diabetes include:
ü Excessive thirst (polydipsia)
ü Polyuria (frequent urination)
ü Unexplained weight loss
ü Fatigue and weakness
ü Blurred vision and headache
ü Slow-healing wounds or frequent infections
ü Numbness or tingling in hands and feet
Reference: https://my.clevelandclinic.org/health/diseases/7104-diabetes
Complications of Uncontrolled Diabetes
This chronic syndrome is usually irreversible, yet with proper management strategies and lifestyle modifications, patients can live a fairly normal life. However, if diabetes remains untreated or poorly controlled, it can lead to serious long-term complications that not only reduce life expectancy but also lower quality of life and place a heavy burden on healthcare systems. It can damage blood vessels and nerves, leading to life-threatening complications such as:
1. Macrovascular Complications:
ü Heart disease (coronary artery disease)
ü Stroke
ü Peripheral vascular disease (poor blood circulation)
2. Microvascular Damage:
ü Diabetic retinopathy (eye damage leading to vision loss)
ü Diabetic nephropathy (kidney damage)
ü Diabetic neuropathy (nerve damage causing numbness, pain, or ulcers)
Diagnostic Criteria of Diabetes:
Regular screening is recommended, especially for those with risk factors. Diagnosis is confirmed through several tests. The diagnostic criteria according to the American Diabetes Association (2023) are as follows:
ü Fasting Blood Glucose Test: This test measures blood sugar after an overnight fast. Fasting plasma glucose (FPG) ≥ 126 mg/dL.
ü HbA1c Test: This shows average blood sugar over the past 2–3 months. HbA1c ≥ 6.5%.
ü Oral Glucose Tolerance Test (OGTT): This test measures the body’s response to sugar intake. 2-hour plasma glucose (OGTT) ≥ 200 mg/dL.
Treatment Options for Diabetes
The treatment options for Diabetes mellitus aim to improve symptoms of hyperglycaemia and minimise the risks of long-term microvascular and macrovascular complications. Managing diabetes requires a multi-pronged approach which includes dietary/ lifestyle modification, oral antidiabetic drugs and injected therapies.
1. Lifestyle Modifications: Modification of lifestyle is one of the most effective strategies to begin with. This includes:
ü Healthy Diet: A healthy diet including whole grains, lean proteins, fresh fruits, and vegetables forms the foundation of diabetes management. Patients are encouraged to reduce the intake of sugary drinks, refined carbohydrates, and processed foods.
ü Exercise: Along with dietary changes, regular physical activity plays a vital role. Moderate-intensity exercise such as brisk walking, swimming, or cycling can significantly improve insulin sensitivity.
ü Weight Management: Obese individuals should work on a modest reduction of 5–10% of body weight; this can make a measurable difference in blood sugar control.
2. Pharmacological Management: For many individuals, pharmacological management becomes necessary. Here’s an overview of the medications available for the management of Diabetes mellitus:
ü Oral Medications: Patients with Type 2 diabetes are often prescribed oral hypoglycemics like metformin which improve insulin sensitivity and lower glucose levels effectively.
ü Insulin Therapy: In advanced Type 2 diabetes cases where oral medications are not enough, or in all cases of Type 1 diabetes, insulin therapy is essential to regulate blood glucose levels.
ü Other Medications: Newer classes of medications, including GLP-1 receptor agonists and SGLT2 inhibitors, not only lower blood sugar but also provide additional benefits such as weight reduction and cardiovascular protection.
3. Monitoring and Regular Check-ups: Regular monitoring and check-ups are crucial.
ü Self-monitoring of blood glucose allows patients to track how well they are managing their condition on a day-to-day basis. HbA1c as a measure of long-term control.
ü Regular visits to healthcare professionals, eye specialists, and kidney function testing are necessary for early detection and management of potential complications.
4. New and Emerging Treatments: In recent years, new and emerging treatments have transformed the management approach of diabetes. Advanced technologies such as artificial pancreas systems, which automatically adjust insulin delivery based on glucose readings, are offering new hope for people with Type 1 diabetes. Furthermore, research into stem cell therapy and gene therapy is opening exciting possibilities for future treatments, with the ultimate goal of restoring the body’s natural ability to produce insulin.
Overall, while Diabetes cannot be cured and is irreversible, the combination of lifestyle changes, medications, ongoing monitoring, and emerging technologies makes it a highly manageable condition, allowing individuals to live healthier and more fulfilling lives.
Conclusion
Diabetes is a chronic metabolic disorder and is a lifelong condition that requires attention, management, monitoring and awareness. With early diagnosis, effective treatment, and lifestyle changes, diabetes can be managed successfully. This allows the patients to live a healthier life and improves the overall quality of life. As research advances, new treatments continue to bring hope for better outcomes. The key lies in awareness, prevention, and consistent management.
Frequently Asked Questions (FAQs)
1. What are the early warning signs of diabetes? Common early signs include frequent urination, excessive thirst, unexplained weight loss, constant fatigue, blurred vision, and slow-healing wounds. If these symptoms appear, then it’s important to get tested.
2. Can diabetes be cured permanently? Currently, diabetes cannot be cured. However, it can be managed effectively with lifestyle changes, medications, and regular monitoring. Some people with Type 2 diabetes may achieve remission with significant weight loss and lifestyle adjustments, but lifelong management is usually required.
3. What foods are contraindicated in diabetic patients? Diabetics should limit sugary drinks, processed foods, refined carbohydrates (like white bread and pastries), and foods high in saturated or trans fats. Instead, focus on whole grains, fresh vegetables, lean proteins, and fiber-rich foods.
4. How often should blood sugar levels be checked? The frequency depends on the type of diabetes and treatment plan. Patients using insulin may need to check multiple times a day, while others might monitor a few times per week. HbA1c tests every 3–6 months are also recommended to track long-term control.
5. What happens if diabetes is left untreated? Untreated or poorly managed diabetes can lead to serious complications, including heart disease, stroke, kidney failure, nerve damage, and vision loss. Early diagnosis and proper management are key to preventing these outcomes.